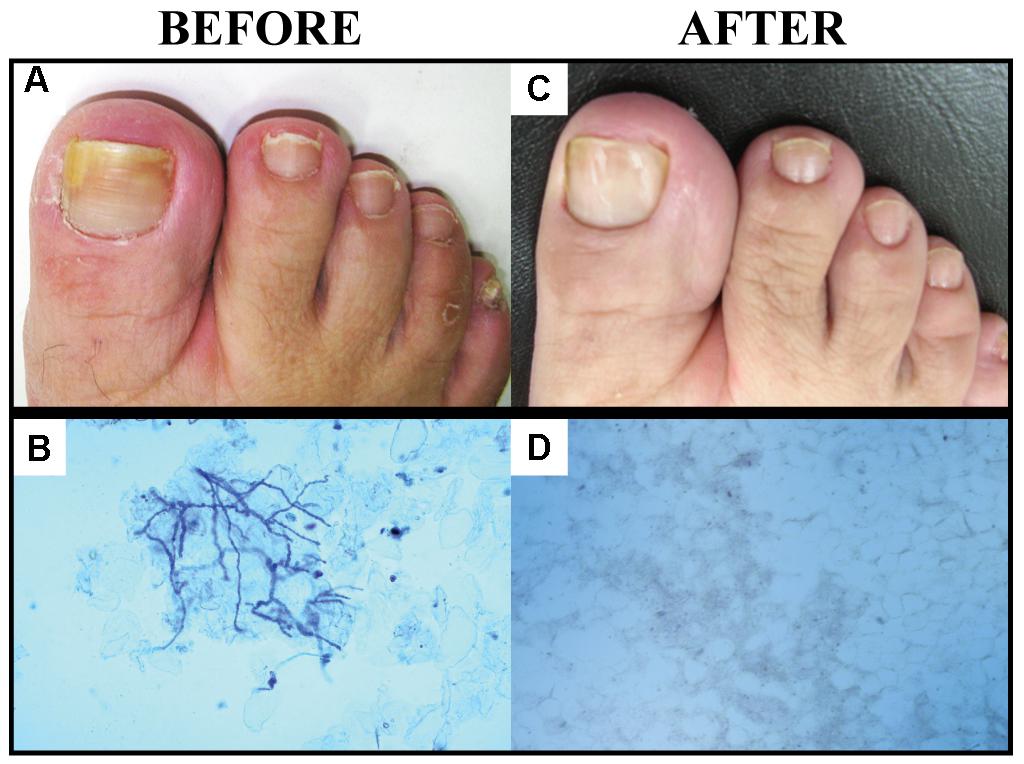
Nail fungal infection, also known as Onychomycosis, is a common condition that affects millions of people worldwide. This type of infection can occur in both fingernails and toenails but is more frequently observed in toenails. It often leads to discoloration, thickening, and crumbling of the nails, causing discomfort and embarrassment for those affected. Understanding the causes, recognizing the symptoms, and exploring treatment options are essential steps toward managing this persistent condition.
What Is Nail Fungal Infection?
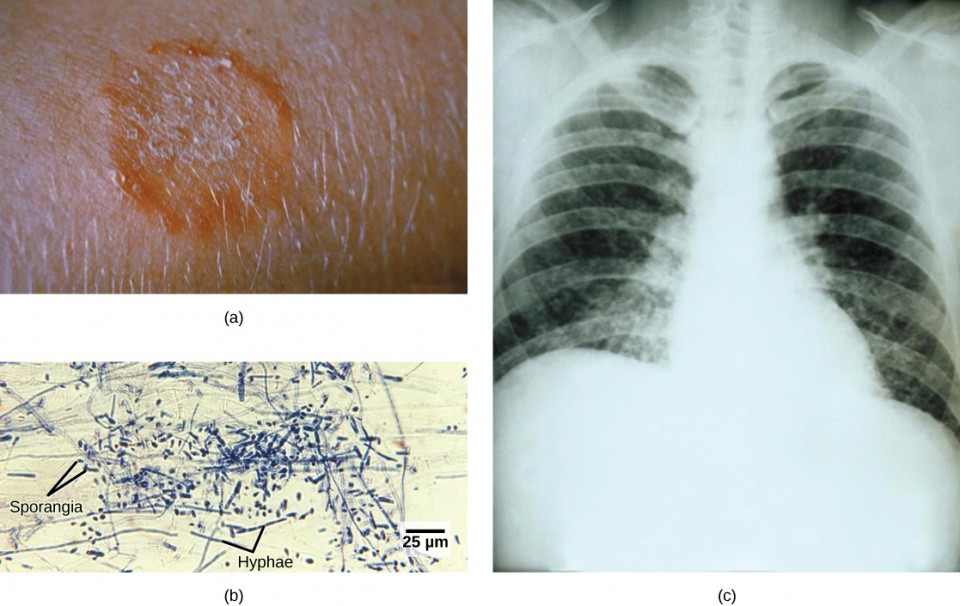
A nail fungal infection occurs when fungi invade the nail bed or the area beneath the nail. These infections are typically caused by dermatophytes, which are a specific group of fungi. However, other types of fungi, such as yeasts and molds, can also contribute to nail infections. The condition often starts as a small spot under the tip of the nail but can spread and worsen over time if left untreated.
How Common Is It?
- Approximately ten percent of adults experience nail fungal infections at some point in their lives.
- The likelihood of developing this condition increases with age, particularly among individuals over sixty years old.
- Toenails are more commonly affected than fingernails due to the warm and moist environment inside shoes, which provides an ideal breeding ground for fungi.
Causes of Nail Fungal Infections
Nail fungal infections occur when fungi enter the nail through small cracks or separations between the nail and the nail bed. Several factors can increase the risk of developing this condition:
1. Environmental Factors
Fungi thrive in warm and damp environments. Public places like swimming pools, locker rooms, and communal showers are common areas where fungi can spread. Walking barefoot in these locations significantly raises the risk of exposure to infectious fungi.
2. Poor Foot Hygiene
Failure to maintain proper foot hygiene can create conditions that promote fungal growth. Wearing sweaty socks or tight-fitting shoes for extended periods can trap moisture, creating an ideal environment for fungi to flourish.
3. Weakened Immune System
Individuals with weakened immune systems, such as those with diabetes, HIV, or undergoing chemotherapy, are more susceptible to nail fungal infections. A compromised immune system makes it harder for the body to fight off fungal invaders.
4. Previous Nail Injuries
Trauma to the nail, whether from an injury or repetitive stress, can damage the nail bed and make it more vulnerable to fungal infections. Even minor injuries can create openings for fungi to enter.
5. Age-Related Changes
As people age, their nails naturally become more brittle and prone to cracking. Additionally, reduced blood circulation in older adults can slow down the body’s ability to heal and resist infections, increasing the likelihood of fungal nail problems.
Symptoms of Nail Fungal Infections
Recognizing the symptoms of nail fungal infections early can help prevent the condition from worsening. Below are the most common signs to watch for:
1. Discoloration
One of the earliest and most noticeable symptoms is a change in the color of the nail. Infected nails may turn yellow, brown, white, or even greenish. In severe cases, the nail may appear dark due to debris buildup underneath.
2. Thickening
Infected nails often become thicker than usual, making them difficult to trim and causing discomfort when wearing shoes. The thickening occurs as the nail tries to protect itself from the invading fungi.
3. Brittle or Crumbly Nails
Fungal infections weaken the structure of the nail, leading to brittleness. Infected nails may crumble easily or break off in pieces, especially at the edges.
4. Distorted Shape
As the infection progresses, the nail may lose its natural shape and develop irregularities. The surface of the nail might appear uneven or warped.
5. Unpleasant Odor
In advanced stages, nail fungal infections can produce a foul smell. This odor is often caused by the breakdown of nail tissue and the presence of fungi and bacteria.
6. Separation from the Nail Bed
In severe cases, the infected nail may lift away from the nail bed, creating a gap where dirt and debris can accumulate. This separation is not only unsightly but also painful.
Risk Factors for Developing Nail Fungal Infections
While anyone can develop a nail fungal infection, certain factors increase the likelihood of contracting the condition:
1. Diabetes
People with diabetes are at a higher risk of developing nail fungal infections due to poor blood circulation and a weakened immune system. Additionally, nerve damage in the feet can reduce sensation, making it harder to notice early signs of infection.
2. Circulatory Problems
Poor blood flow to the extremities can impair the body’s ability to fight off infections, including those affecting the nails.
3. Heavy Sweating
Excessive sweating creates a moist environment that encourages fungal growth. Individuals who sweat heavily, especially on their feet, are more prone to developing nail infections.
4. Living in Humid Climates
Residing in areas with high humidity levels increases the risk of exposure to fungi, as these organisms thrive in damp conditions.
5. Sharing Personal Items
Sharing items like nail clippers, towels, or shoes with an infected person can lead to the transmission of fungi. Proper hygiene practices and avoiding shared personal items can help reduce this risk.
Treatment Options for Nail Fungal Infections
Treating nail fungal infections can be challenging, as the nails grow slowly and the infection often penetrates deep into the nail bed. However, several treatment options are available to manage and eliminate the condition:
1. Topical Antifungal Medications
Topical treatments are applied directly to the affected nail. These medications come in the form of creams, ointments, or nail lacquers. While they are easy to use, topical treatments may take several months to show results because nails grow slowly.
2. Oral Antifungal Medications
Oral medications are often prescribed for more severe cases of nail fungal infections. These drugs work by targeting the fungi from within the body. Common oral antifungal medications include terbinafine and itraconazole. While effective, these medications can have side effects and may not be suitable for everyone, especially individuals with liver problems.
3. Laser Therapy
Laser treatment is a newer option for addressing nail fungal infections. During this procedure, a laser beam is used to target and destroy the fungi without damaging the surrounding tissue. Laser therapy is generally considered safe, but multiple sessions may be required for optimal results.
4. Surgical Removal of the Nail
In extreme cases where the infection is severe and does not respond to other treatments, surgical removal of the nail may be necessary. This procedure allows direct access to the nail bed for treatment and enables a new, healthy nail to grow in its place.
5. Home Remedies
Some individuals opt for home remedies to manage mild cases of nail fungal infections. Popular options include applying tea tree oil, vinegar soaks, or baking soda pastes to the affected area. While these remedies may provide temporary relief, they are not scientifically proven to cure the infection completely.
Preventing Nail Fungal Infections
Taking preventive measures can significantly reduce the risk of developing nail fungal infections. Here are some practical tips:
1. Keep Nails Clean and Dry
Regularly washing and thoroughly drying your hands and feet can help prevent fungi from taking hold. Pay special attention to drying between the toes after bathing or swimming.
2. Wear Breathable Footwear
Choose shoes made from breathable materials like leather or mesh to allow air circulation and reduce moisture buildup. Avoid wearing tight or poorly ventilated shoes for extended periods.
3. Use Antifungal Powders or Sprays
Applying antifungal powders or sprays inside your shoes can help kill any fungi present and prevent reinfection.
4. Avoid Walking Barefoot in Public Areas
Always wear protective footwear, such as flip-flops, in public showers, locker rooms, and pool areas to minimize exposure to fungi.
5. Trim Nails Regularly
Keeping your nails short and well-trimmed reduces the risk of fungi entering through cracks or separations. Use clean, sterilized tools to avoid spreading infections.
6. Maintain a Healthy Lifestyle
A strong immune system plays a crucial role in preventing infections. Eating a balanced diet, exercising regularly, and getting enough sleep can help boost your body’s defenses against fungi.
When to See a Doctor
If you suspect you have a nail fungal infection, it is important to seek medical advice, especially if the condition does not improve with over-the-counter treatments. A healthcare professional can confirm the diagnosis and recommend appropriate treatment options based on the severity of the infection. Early intervention can prevent complications and improve outcomes.