Meningitis, often abbreviated as “mening.,” is a serious medical condition that involves the inflammation of the protective membranes surrounding the brain and spinal cord, known as the meninges. This condition can arise from various causes, including infections, injuries, or other underlying health issues. Meningitis demands immediate attention due to its potential to cause severe complications or even death if left untreated. In this article, we will explore the intricacies of this condition, its causes, symptoms, diagnosis, treatment options, and preventive measures.
What Are the Meninges?
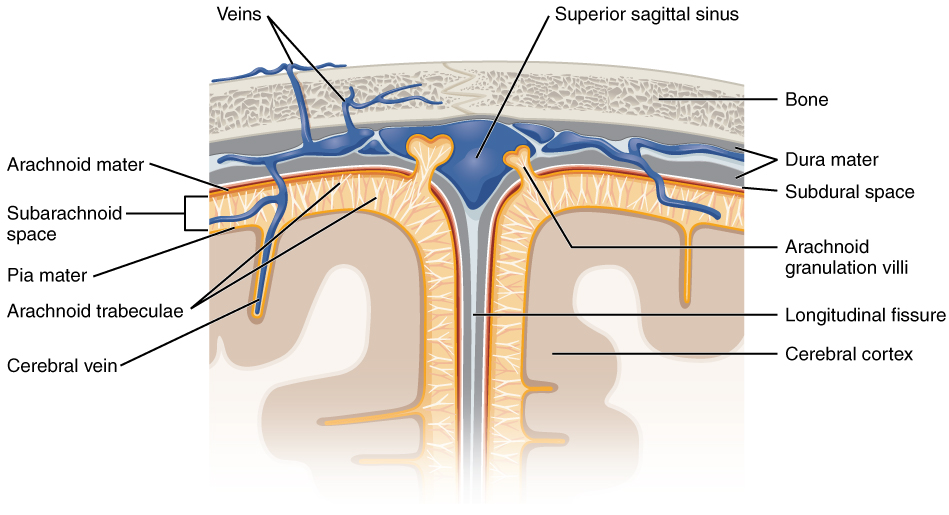
The meninges are three layers of protective tissue that surround the brain and spinal cord. These layers play a crucial role in safeguarding the central nervous system from external harm. The three layers are:
- Dura mater: The outermost layer, which is tough and fibrous.
- Arachnoid mater: The middle layer, characterized by a web-like structure.
- Pia mater: The innermost layer, which is delicate and closely adheres to the surface of the brain and spinal cord.
When these layers become inflamed, it disrupts their ability to protect the central nervous system, leading to the condition known as meningitis.
Causes of Meningitis
Meningitis can be caused by a variety of factors, with infections being the most common. Below are the primary causes of this condition:
Infectious Causes
Infections are the leading cause of meningitis and can result from bacteria, viruses, fungi, or parasites. Each type of infection has distinct characteristics:
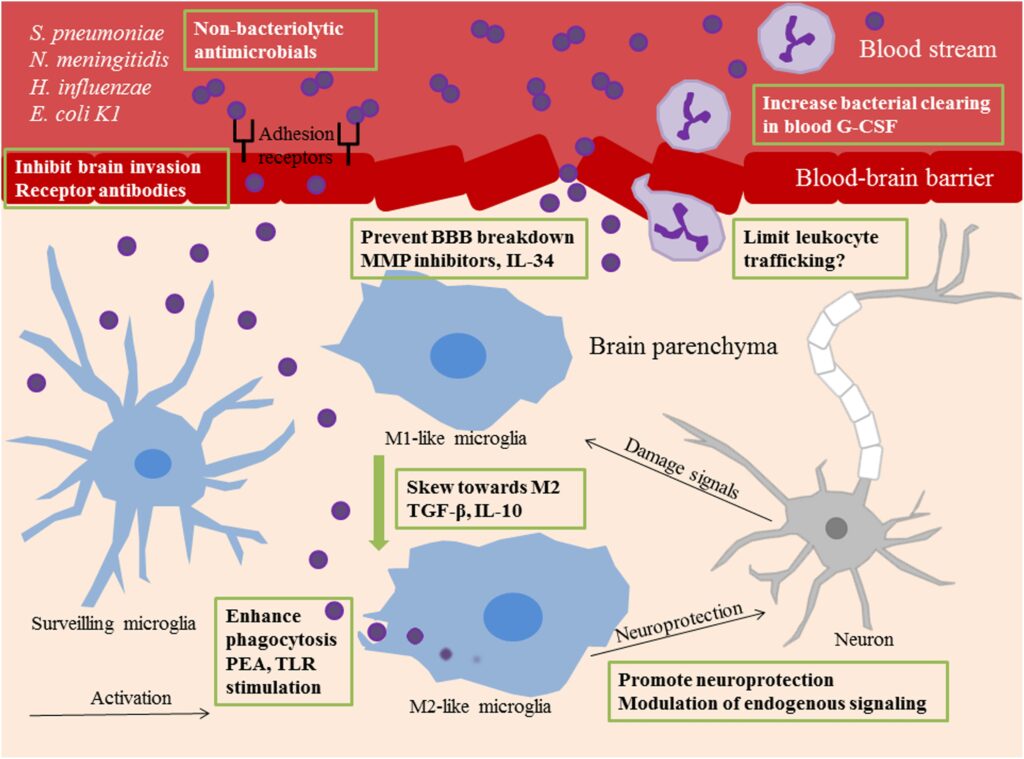
- Bacterial meningitis: This form is often life-threatening and requires urgent medical intervention. Common bacteria responsible for bacterial meningitis include Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae.
- Viral meningitis: Generally less severe than bacterial meningitis, viral meningitis is often caused by enteroviruses. It tends to resolve on its own with supportive care.
- Fungal meningitis: This type is rare but can occur in individuals with weakened immune systems, such as those with HIV or cancer. Cryptococcus is a common fungal culprit.
- Parasitic meningitis: Caused by parasites, this form is extremely rare but can be severe. Naegleria fowleri, a waterborne parasite, is an example.
Non-Infectious Causes
In addition to infections, meningitis can also result from non-infectious factors, including:
- Head injuries: Trauma to the head or spine can lead to inflammation of the meninges.
- Certain medications: Some drugs, particularly those used in chemotherapy or immunosuppressive therapy, can trigger inflammation.
- Cancer: Tumors that spread to the central nervous system can cause irritation and inflammation of the meninges.
- Autoimmune disorders: Conditions like lupus or rheumatoid arthritis can lead to inflammation of the meninges.
Symptoms of Meningitis
The symptoms of meningitis can vary depending on the cause and the age of the individual. However, some common signs and symptoms include:
- Fever: A high body temperature is one of the hallmark symptoms of meningitis.
- Severe headache: The headache associated with meningitis is often described as intense and unrelenting.
- Stiff neck: Difficulty bending the neck forward is a classic sign of meningitis.
- Nausea and vomiting: These symptoms may accompany the headache and fever.
- Sensitivity to light: Many individuals with meningitis experience photophobia, or discomfort in bright light.
- Confusion or altered mental state: This can range from mild confusion to severe disorientation or even coma.
- Rash: In cases of bacterial meningitis caused by certain bacteria, a distinctive rash may appear.
In infants, symptoms may differ and can include irritability, poor feeding, lethargy, and a bulging fontanelle (soft spot on the skull).
Diagnosing Meningitis
Diagnosing meningitis involves a combination of clinical evaluation, laboratory tests, and imaging studies. Prompt diagnosis is essential to initiate appropriate treatment. The diagnostic process typically includes:
Medical History and Physical Examination
A healthcare provider will begin by taking a detailed medical history and performing a physical examination. They will assess symptoms such as fever, headache, and neck stiffness, and look for signs of infection or other underlying conditions.
Lumbar Puncture
A lumbar puncture, also known as a spinal tap, is a critical diagnostic procedure for meningitis. During this procedure, a small sample of cerebrospinal fluid is collected from the spinal canal. The fluid is then analyzed in a laboratory to determine the presence of infection, inflammation, or other abnormalities.
Imaging Studies
In some cases, imaging studies such as computed tomography (CT) scans or magnetic resonance imaging (MRI) may be performed to rule out other causes of symptoms, such as brain tumors or abscesses.
Blood Tests
Blood tests can help identify infections or inflammatory markers that may indicate meningitis. These tests can also assist in determining the specific pathogen causing the condition.
Treatment Options for Meningitis
The treatment of meningitis depends on its underlying cause. Early and appropriate treatment is crucial to prevent complications and improve outcomes.
Treatment for Bacterial Meningitis
Bacterial meningitis is a medical emergency and requires immediate treatment with antibiotics. The choice of antibiotic depends on the specific bacteria causing the infection. In some cases, corticosteroids may also be administered to reduce inflammation and prevent complications such as hearing loss.
Treatment for Viral Meningitis
Viral meningitis is typically managed with supportive care, as it often resolves on its own. This may include rest, hydration, pain relievers, and medications to reduce fever. Antiviral medications may be prescribed in rare cases, such as when herpes simplex virus is the cause.
Treatment for Fungal Meningitis
Fungal meningitis is treated with antifungal medications. The duration of treatment can be lengthy, often lasting several weeks to months, depending on the severity of the infection and the patient’s response to therapy.
Treatment for Non-Infectious Meningitis
For non-infectious meningitis, treatment focuses on addressing the underlying cause. For example, stopping a medication that triggered the inflammation or managing an autoimmune disorder with immunosuppressive drugs may be necessary.
Preventing Meningitis
Preventive measures can significantly reduce the risk of developing meningitis. Some key strategies include:
Vaccination
Vaccines are available to protect against several types of bacterial meningitis, including those caused by Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Routine vaccination schedules for children and adolescents include these vaccines, and booster doses may be recommended for adults at higher risk.
Practicing Good Hygiene
Good hygiene practices, such as regular handwashing, can help prevent the spread of viruses and bacteria that cause meningitis. Avoiding close contact with individuals who are sick is also advisable.
Avoiding Risky Behaviors
Certain behaviors, such as sharing utensils or engaging in unprotected sexual activity, can increase the risk of contracting infections that lead to meningitis. Taking precautions can help minimize these risks.
Managing Underlying Health Conditions
Individuals with weakened immune systems should work closely with their healthcare providers to manage their conditions and reduce the risk of infections that could lead to meningitis.