Osteoarthritis, often abbreviated as OA, is one of the most common forms of arthritis that affects millions of people worldwide. It is a degenerative joint disease that primarily impacts the cartilage, the smooth tissue covering the ends of bones in joints. Over time, this condition can lead to pain, stiffness, and reduced mobility, significantly affecting a person’s quality of life. This article will delve into the causes, symptoms, diagnosis methods, and available treatment options for osteoarthritis.
What Causes Osteoarthritis?
Osteoarthritis develops when the protective cartilage that cushions the ends of bones wears down over time. While the exact cause of this condition is not fully understood, several factors are known to contribute to its development:
Age
As people grow older, their risk of developing osteoarthritis increases. The wear and tear on joints accumulate over the years, making age one of the primary risk factors.
Obesity
Excess body weight places additional stress on weight-bearing joints such as the knees, hips, and spine. This added pressure accelerates the breakdown of cartilage, increasing the likelihood of osteoarthritis.
Injury or Overuse
Previous injuries to joints, such as fractures or ligament tears, can predispose individuals to osteoarthritis later in life. Similarly, repetitive movements or overuse of certain joints, often seen in athletes or those with physically demanding jobs, can also contribute to the condition.
Genetics
Some people inherit a predisposition to osteoarthritis. Genetic factors can affect the durability of cartilage or the overall structure of joints, making them more susceptible to damage.
Joint Misalignment
Abnormalities in joint structure, such as bowed legs or uneven leg lengths, can place uneven stress on joints. This imbalance can accelerate cartilage breakdown and lead to osteoarthritis.
Other Medical Conditions
Certain medical conditions, such as rheumatoid arthritis or metabolic disorders like hemochromatosis, can increase the risk of developing osteoarthritis. These conditions may directly affect joint health or contribute to inflammation that damages cartilage.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis typically develop gradually and worsen over time. They vary depending on the affected joints but commonly include the following:
Pain
Persistent pain in the affected joints is one of the hallmark symptoms of osteoarthritis. The pain often worsens with activity and improves with rest. In advanced stages, the pain may persist even during periods of inactivity.
Stiffness
Joint stiffness is another common symptom, particularly after periods of inactivity. Many individuals experience stiffness upon waking up in the morning or after sitting for extended periods. This stiffness usually lasts for a short duration but can be bothersome.
Reduced Flexibility
As osteoarthritis progresses, the affected joints may lose their range of motion. Individuals may find it challenging to perform everyday tasks that require bending, twisting, or stretching.
Swelling
Soft tissue inflammation around the affected joints can lead to swelling. This symptom is often accompanied by tenderness and discomfort when pressing on or moving the joint.
Grating Sensation
Some people with osteoarthritis report hearing or feeling a grating sensation when moving the affected joint. This occurs due to the roughening of cartilage surfaces or the presence of bone spurs, which are small bony projections that develop along joint edges.
Bone Spurs
Bone spurs themselves may not always cause symptoms, but they can contribute to joint pain and stiffness by altering the joint’s structure and function.
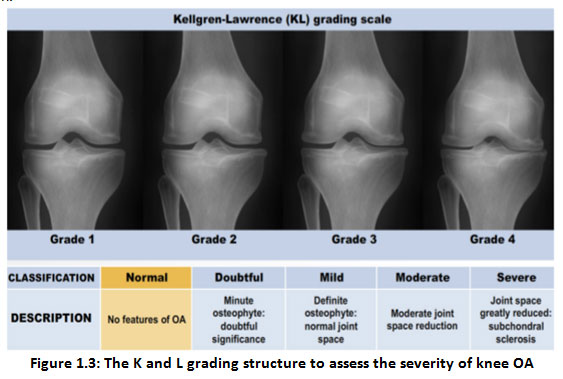
Diagnosing Osteoarthritis
Diagnosing osteoarthritis involves a combination of clinical evaluation, imaging tests, and sometimes laboratory tests. Healthcare providers use these tools to rule out other potential causes of joint pain and confirm the presence of osteoarthritis.
Medical History and Physical Examination
A healthcare provider will begin by taking a detailed medical history, asking about symptoms, their duration, and any factors that worsen or alleviate the pain. During the physical examination, the provider will assess the affected joints for signs of swelling, tenderness, and reduced range of motion.
Imaging Tests
Imaging tests play a crucial role in diagnosing osteoarthritis. Commonly used imaging techniques include:
- X-rays: X-rays can reveal cartilage loss, narrowing of joint spaces, and the presence of bone spurs. These findings help confirm the diagnosis and determine the severity of the condition.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of soft tissues, including cartilage, tendons, and ligaments. While not routinely required, MRI may be used to gain further insight into joint damage.
Laboratory Tests
Although there are no specific blood tests for osteoarthritis, laboratory tests may be conducted to rule out other forms of arthritis, such as rheumatoid arthritis or gout. These tests may include:
- Blood Tests: Blood tests can detect markers of inflammation or autoimmune conditions.
- Joint Fluid Analysis: In some cases, fluid may be extracted from the affected joint to check for signs of infection, inflammation, or crystal deposits, which could indicate other types of arthritis.
Treatment Options for Osteoarthritis
While there is no cure for osteoarthritis, various treatment options can help manage symptoms, improve joint function, and enhance quality of life. The choice of treatment depends on the severity of the condition, the affected joints, and the individual’s overall health.
Lifestyle Modifications
Adopting healthy lifestyle habits can significantly reduce the impact of osteoarthritis. Some effective strategies include:
- Weight Management: Losing excess weight reduces stress on weight-bearing joints, alleviating pain and slowing disease progression.
- Exercise: Low-impact activities such as swimming, cycling, and walking can strengthen muscles around the joints, improve flexibility, and reduce pain.
- Dietary Changes: Consuming anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, may help reduce joint inflammation.
Medications
Several medications are available to relieve pain and inflammation associated with osteoarthritis. These include:
- Over-the-Counter Pain Relievers: Acetaminophen and nonsteroidal anti-inflammatory drugs, such as ibuprofen, are commonly used to manage mild to moderate pain.
- Topical Treatments: Creams or ointments containing capsaicin or nonsteroidal anti-inflammatory agents can provide localized relief.
- Prescription Medications: In cases of severe pain, stronger prescription medications may be necessary.
Physical Therapy
Physical therapy focuses on strengthening the muscles surrounding the affected joints, improving flexibility, and enhancing overall joint function. A physical therapist can design a personalized exercise program tailored to an individual’s needs.
Assistive Devices
Using assistive devices, such as braces, splints, or canes, can help reduce stress on damaged joints and improve mobility. These devices provide support and stability, allowing individuals to perform daily activities more comfortably.
Injections
For individuals with moderate to severe osteoarthritis, injections may offer temporary relief. Common injection options include:
- Corticosteroids: These powerful anti-inflammatory medications are injected directly into the joint to reduce pain and swelling.
- Hyaluronic Acid: This substance mimics the natural lubricant found in joints, potentially improving joint function and reducing pain.
Surgical Interventions
In advanced cases where conservative treatments fail to provide relief, surgery may be considered. Surgical options include:
- Arthroscopy: A minimally invasive procedure used to remove loose cartilage or repair damaged tissues.
- Osteotomy: This procedure involves realigning bones to redistribute stress away from the damaged area of the joint.
- Joint Replacement Surgery: Also known as arthroplasty, this surgery involves replacing the damaged joint with an artificial one, typically made of metal or plastic components.
Alternative Therapies
Some individuals explore alternative therapies to complement traditional treatments. These may include:
- Acupuncture: This ancient practice involves inserting thin needles into specific points on the body to relieve pain.
- Massage Therapy: Massaging the muscles around the affected joints can reduce tension and improve circulation.
- Herbal Supplements: Certain supplements, such as glucosamine and chondroitin, are believed to support joint health, though scientific evidence supporting their effectiveness is mixed.
Preventing Osteoarthritis
While not all cases of osteoarthritis can be prevented, adopting preventive measures can reduce the risk or delay the onset of the condition. Key strategies include maintaining a healthy weight, engaging in regular physical activity, avoiding joint injuries, and using proper techniques when lifting heavy objects or performing repetitive tasks.