Orchitis, commonly referred to as testicle inflammation, is a condition that affects the male reproductive system. It involves swelling and pain in one or both testicles, often caused by an infection or injury. This condition can lead to complications if left untreated, making it essential to understand its causes, symptoms, diagnosis methods, and treatment options.
What Is Orchitis?
Orchitis is the medical term for inflammation of the testicles. The testicles are vital organs responsible for producing sperm and testosterone, and any disruption to their function can have significant effects on fertility and overall health. While orchitis can occur at any age, it is most commonly seen in adolescents and adults.
Types of Orchitis
- Viral Orchitis: Often associated with viral infections like mumps.
- Bacterial Orchitis: Usually linked to urinary tract infections or sexually transmitted infections.
Causes of Orchitis
The causes of orchitis can vary depending on whether the condition is viral or bacterial. Understanding these causes is crucial for prevention and effective treatment.
Viral Causes
Viral orchitis is most frequently caused by the mumps virus. Mumps is a contagious disease that primarily affects the salivary glands but can also spread to the testicles, especially in post-pubertal males. When the mumps virus infects the testicles, it triggers an inflammatory response, leading to orchitis.
Bacterial Causes
Bacterial orchitis is often a complication of other infections. Some common sources include:
- Urinary Tract Infections: Bacteria from the urinary tract can travel to the testicles, causing inflammation.
- Sexually Transmitted Infections: Infections such as gonorrhea and chlamydia can lead to epididymitis, which may progress to orchitis.
- Prostate Infections: Bacteria from an infected prostate gland can spread to the testicles.
Other Potential Causes
In rare cases, orchitis can result from trauma to the testicles or autoimmune disorders where the body’s immune system mistakenly attacks the testicular tissue.
Symptoms of Orchitis
Recognizing the symptoms of orchitis is essential for early diagnosis and treatment. The symptoms can vary depending on the underlying cause but generally include the following:
Common Symptoms
- Swelling of one or both testicles
- Pain or discomfort in the scrotum
- Redness or warmth in the scrotal area
- Fever and chills
- Nausea and vomiting
- Pain during urination
- Abnormal discharge from the penis
Symptoms Specific to Viral Orchitis
Viral orchitis caused by mumps typically occurs about four to seven days after the onset of parotitis, which is the swelling of the salivary glands. In addition to the common symptoms, individuals may experience:
- Swollen salivary glands
- Headache
- Muscle aches
Diagnosis of Orchitis
Diagnosing orchitis involves a combination of physical examination, medical history review, and diagnostic tests. A healthcare provider will assess the symptoms and perform specific evaluations to determine the underlying cause.
Physical Examination
A doctor will conduct a thorough physical examination of the scrotum to check for swelling, tenderness, and redness. They may also examine the abdomen and groin area to rule out other conditions.
Medical History Review
Understanding the patient’s medical history is critical. The doctor will ask about recent illnesses, sexual activity, and any history of urinary tract or sexually transmitted infections.
Diagnostic Tests
To confirm the diagnosis and identify the cause of orchitis, several tests may be performed:
- Urine Analysis: To detect signs of infection in the urinary tract.
- Blood Tests: To check for elevated white blood cell counts or specific antibodies related to infections like mumps.
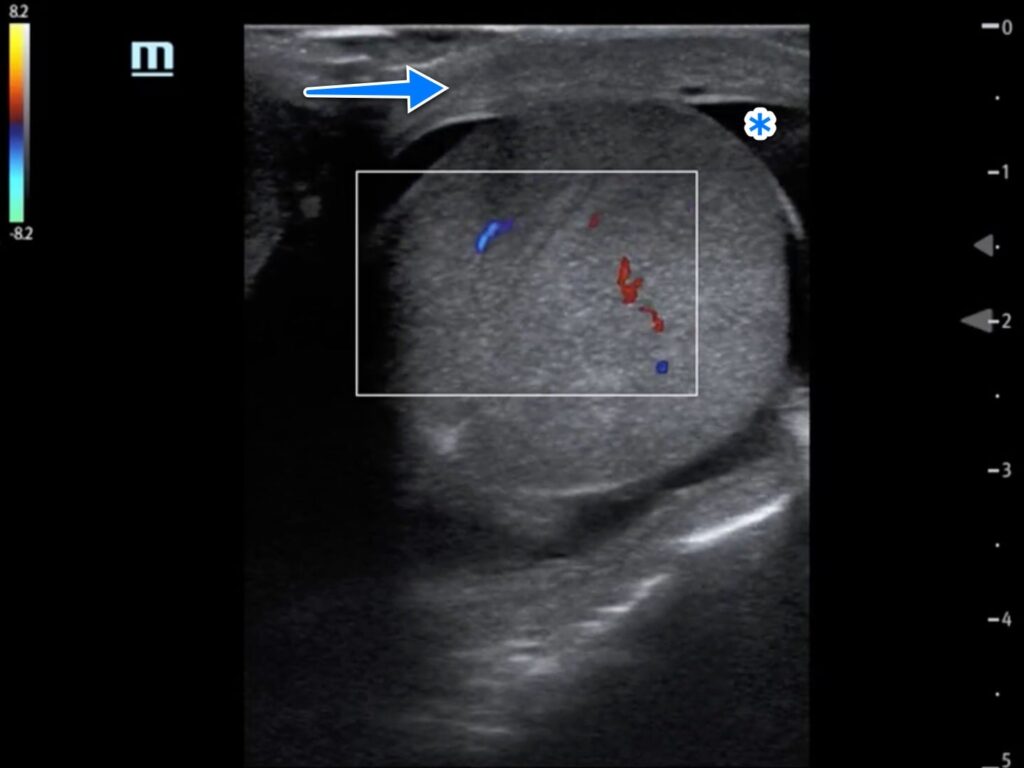
- Ultrasound: An imaging test to evaluate the structure of the testicles and rule out other conditions such as testicular torsion.
- STI Testing: If a sexually transmitted infection is suspected, samples may be taken for laboratory analysis.
Treatment Options for Orchitis
The treatment for orchitis depends on its underlying cause. Both viral and bacterial orchitis require different approaches, and early intervention is key to preventing complications.
Treatment for Viral Orchitis
Viral orchitis, particularly when caused by mumps, does not have a specific cure. However, supportive care can help manage the symptoms:
- Rest: Avoid strenuous activities and allow the body to recover.
- Cold Compresses: Applying ice packs to the scrotum can reduce swelling and pain.
- Pain Relievers: Over-the-counter medications like ibuprofen can alleviate discomfort.
- Elevation: Supporting the scrotum with snug underwear or a jockstrap can provide relief.
Treatment for Bacterial Orchitis
Bacterial orchitis requires antibiotic therapy to eliminate the infection. The choice of antibiotics depends on the specific bacteria causing the infection:
- Antibiotics: Commonly prescribed antibiotics include ceftriaxone and doxycycline. It is crucial to complete the full course of antibiotics even if symptoms improve.
- Rest and Support: Similar to viral orchitis, rest and scrotal support are recommended.
- Follow-Up: Regular follow-up appointments ensure the infection is resolving and prevent complications.
Treatment for Complications
If orchitis leads to complications such as abscess formation or infertility, additional treatments may be necessary:
- Drainage: Abscesses may require surgical drainage.
- Hormonal Therapy: In cases of reduced testosterone production, hormone replacement therapy may be considered.
Preventing Orchitis
While not all cases of orchitis can be prevented, certain measures can reduce the risk:
- Vaccination: The mumps vaccine is part of the routine childhood immunization schedule and significantly reduces the risk of viral orchitis.
- Safe Sexual Practices: Using condoms and practicing safe sex can lower the risk of sexually transmitted infections that may lead to bacterial orchitis.
- Hygiene: Maintaining good personal hygiene can help prevent urinary tract infections.
- Prompt Treatment: Addressing urinary tract or prostate infections promptly can prevent them from spreading to the testicles.
When to Seek Medical Attention
It is important to seek medical attention if you experience any of the following:
- Severe pain or swelling in the testicles
- Fever or chills accompanying testicular pain
- Signs of infection such as pus or abnormal discharge
- Persistent symptoms despite home care
Early diagnosis and treatment can prevent complications such as infertility, abscess formation, or chronic pain.