Optic neuritis, often abbreviated as ON, is a condition characterized by inflammation of the optic nerve. The optic nerve plays a crucial role in transmitting visual information from the eyes to the brain. When this nerve becomes inflamed, it can lead to temporary vision loss and other symptoms that may significantly impact a person’s quality of life. This article delves into the causes, symptoms, diagnosis, and treatment options for this condition.
Understanding the Optic Nerve
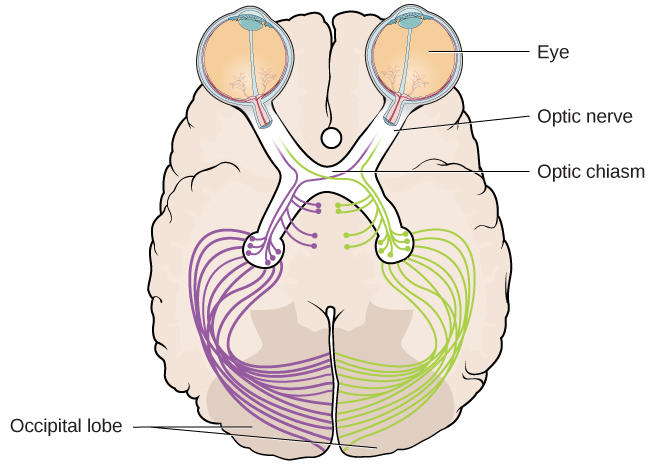
The optic nerve is a bundle of more than one million nerve fibers that connect the retina of the eye to the brain. It serves as the primary pathway for visual information, enabling us to perceive the world around us. Any damage or inflammation to this nerve can disrupt the transmission of visual signals, leading to impaired vision.
What Happens During Inflammation?
Inflammation of the optic nerve occurs when the immune system mistakenly attacks the protective covering of the nerve fibers, known as myelin. This attack can cause swelling and damage, disrupting the normal flow of visual information. The inflammation can occur in one or both eyes, though it typically affects only one eye at a time.
Causes of Optic Neuritis
The exact cause of optic neuritis is not always clear, but several factors and underlying conditions are known to contribute to its development. Below are some of the most common causes:
Autoimmune Disorders
- Multiple Sclerosis: This is one of the most well-known causes of optic neuritis. Multiple sclerosis is a chronic autoimmune disease where the immune system attacks the central nervous system, including the optic nerve.
- Neuromyelitis Optica: Also known as Devic’s disease, this condition specifically targets the optic nerves and spinal cord, leading to severe inflammation and damage.
Infections
- Viral Infections: Certain viral infections, such as measles, mumps, and herpes, have been linked to the development of optic neuritis.
- Bacterial Infections: In rare cases, bacterial infections like Lyme disease or tuberculosis can trigger inflammation of the optic nerve.
Other Factors
- Medications: Some medications, particularly those used in chemotherapy, can increase the risk of developing optic neuritis as a side effect.
- Environmental Triggers: Exposure to certain toxins or chemicals may also contribute to the onset of this condition.
Symptoms of Optic Neuritis
The symptoms of optic neuritis can vary depending on the severity of the inflammation and the individual affected. However, there are several hallmark signs that are commonly reported by patients:
Vision Loss
One of the most noticeable symptoms is a sudden decrease in vision. This vision loss is often described as blurred or dimmed vision and typically affects one eye. In some cases, individuals may experience complete vision loss in the affected eye, though this is usually temporary.
Pain with Eye Movement
Many people with optic neuritis report pain when moving their eyes. This discomfort is caused by the inflammation affecting the nerve and surrounding tissues. The pain is often described as a dull ache or sharp sensation and tends to worsen with eye movement.
Loss of Color Vision
Patients may notice that colors appear less vibrant or washed out. This symptom, known as dyschromatopsia, is a result of the impaired transmission of visual signals through the inflamed optic nerve.
Flashing Lights or Visual Disturbances
Some individuals may experience flashes of light or unusual visual disturbances, such as seeing spots or floaters. These symptoms can be alarming and may indicate significant inflammation of the nerve.
Diagnosing Optic Neuritis
Diagnosing optic neuritis requires a thorough evaluation by an eye care professional. Several diagnostic tools and tests are used to confirm the presence of inflammation and rule out other potential causes of vision problems.
Clinical Examination
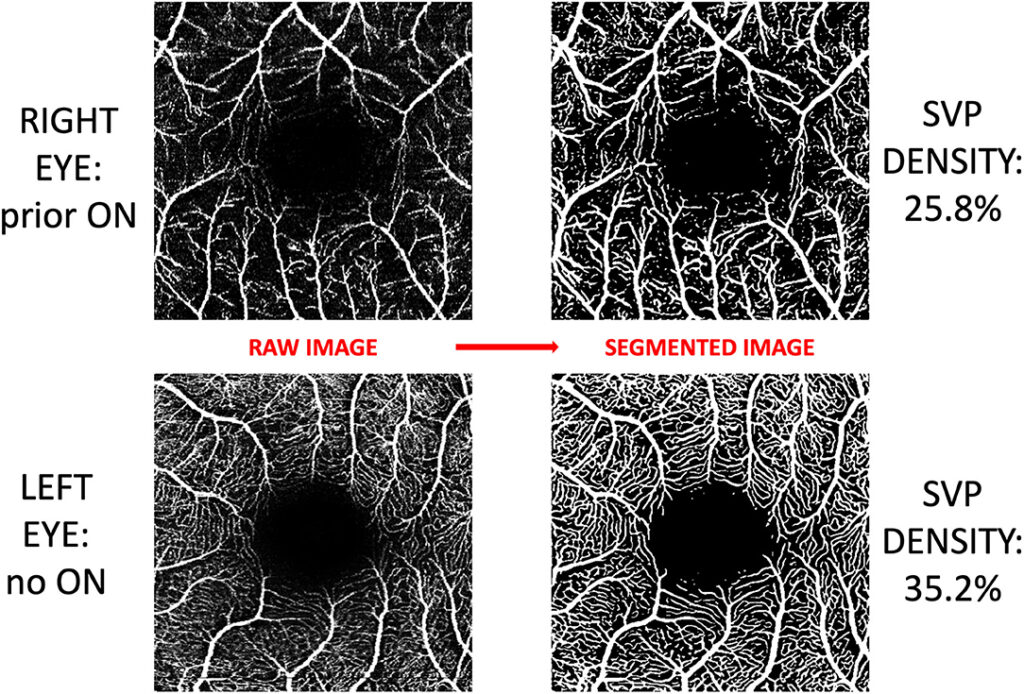
The first step in diagnosing optic neuritis involves a comprehensive eye examination. During this exam, the doctor will assess the patient’s vision, check for color vision abnormalities, and evaluate the reaction of the pupils to light.
Magnetic Resonance Imaging
Magnetic resonance imaging, commonly referred to as MRI, is a key diagnostic tool used to detect inflammation or lesions along the optic nerve. An MRI can also help identify whether the condition is associated with multiple sclerosis or other neurological disorders.
Visual Evoked Potentials
This test measures the electrical activity in the brain in response to visual stimuli. Slowed responses during a visual evoked potentials test can indicate damage to the optic nerve, supporting a diagnosis of optic neuritis.
Lumbar Puncture
In some cases, a lumbar puncture, or spinal tap, may be performed to analyze the cerebrospinal fluid. Elevated levels of certain proteins or immune cells in the fluid can provide additional evidence of inflammation and help guide treatment decisions.
Treatment Options for Optic Neuritis
While optic neuritis often resolves on its own over time, treatment is available to speed up recovery and reduce the risk of complications. The choice of treatment depends on the underlying cause and severity of the condition.
Steroid Therapy
High-dose intravenous corticosteroids are the most common treatment for optic neuritis. These medications work by reducing inflammation and suppressing the immune system’s response. Steroid therapy can help restore vision more quickly and minimize the risk of long-term damage to the optic nerve.
Plasma Exchange Therapy
For patients who do not respond well to steroid therapy, plasma exchange therapy may be considered. This procedure involves removing harmful antibodies and inflammatory substances from the blood, which can help alleviate symptoms and promote healing.
Treating Underlying Conditions
If optic neuritis is caused by an underlying condition such as multiple sclerosis or an infection, treating the root cause is essential. For example, medications that modify the immune system may be prescribed for individuals with multiple sclerosis to prevent future episodes of optic neuritis.
Lifestyle Modifications
In addition to medical treatments, certain lifestyle changes can support recovery and improve overall eye health. These include:
- Avoiding smoking, as it can exacerbate inflammation and delay healing.
- Eating a balanced diet rich in antioxidants to support nerve health.
- Protecting the eyes from bright lights and excessive strain during recovery.
Prognosis and Recovery
The prognosis for individuals with optic neuritis is generally favorable, with most people experiencing significant improvement in their vision within weeks to months. However, the extent of recovery can vary depending on factors such as the severity of the inflammation and the presence of underlying conditions.
Potential Complications
While many patients recover fully, some may experience residual effects, such as mild vision loss or difficulty distinguishing colors. In rare cases, recurrent episodes of optic neuritis can lead to permanent vision impairment.
Monitoring and Follow-Up
Regular follow-up appointments with an eye care professional are essential to monitor progress and detect any signs of recurring inflammation. Early intervention can help prevent further damage and ensure the best possible outcome.