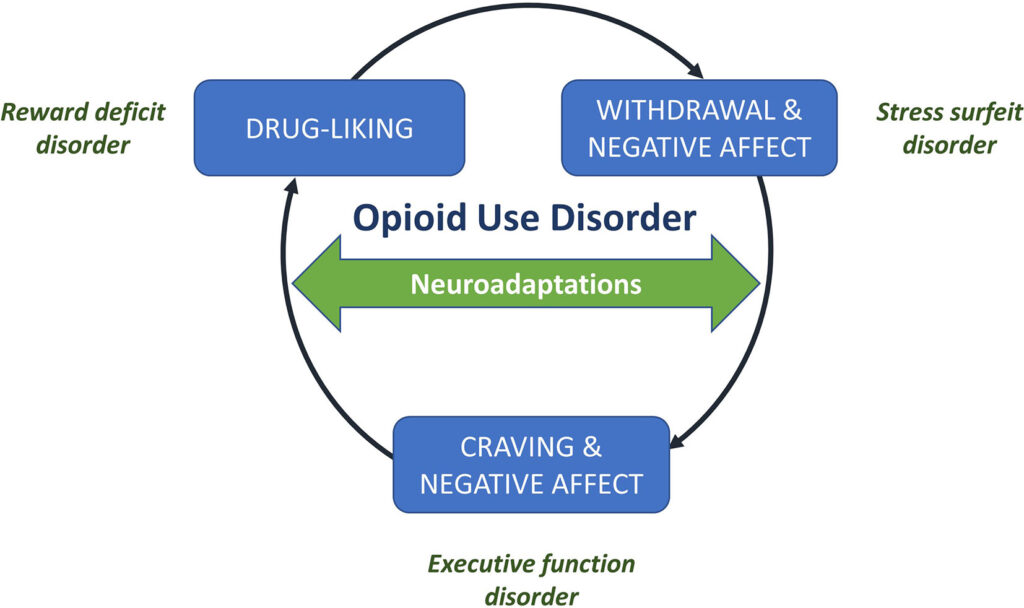
Opioid withdrawal is a challenging process that individuals face when they stop using opioids after prolonged use. Opioids, which include prescription painkillers and illegal substances like heroin, can lead to physical dependence. When someone dependent on these substances reduces or stops their intake, the body reacts with a range of symptoms known as opioid withdrawal syndrome (OWS). Understanding the symptoms, timeline, and management strategies for opioid withdrawal is crucial for those affected and their caregivers.
What Happens During Opioid Withdrawal?
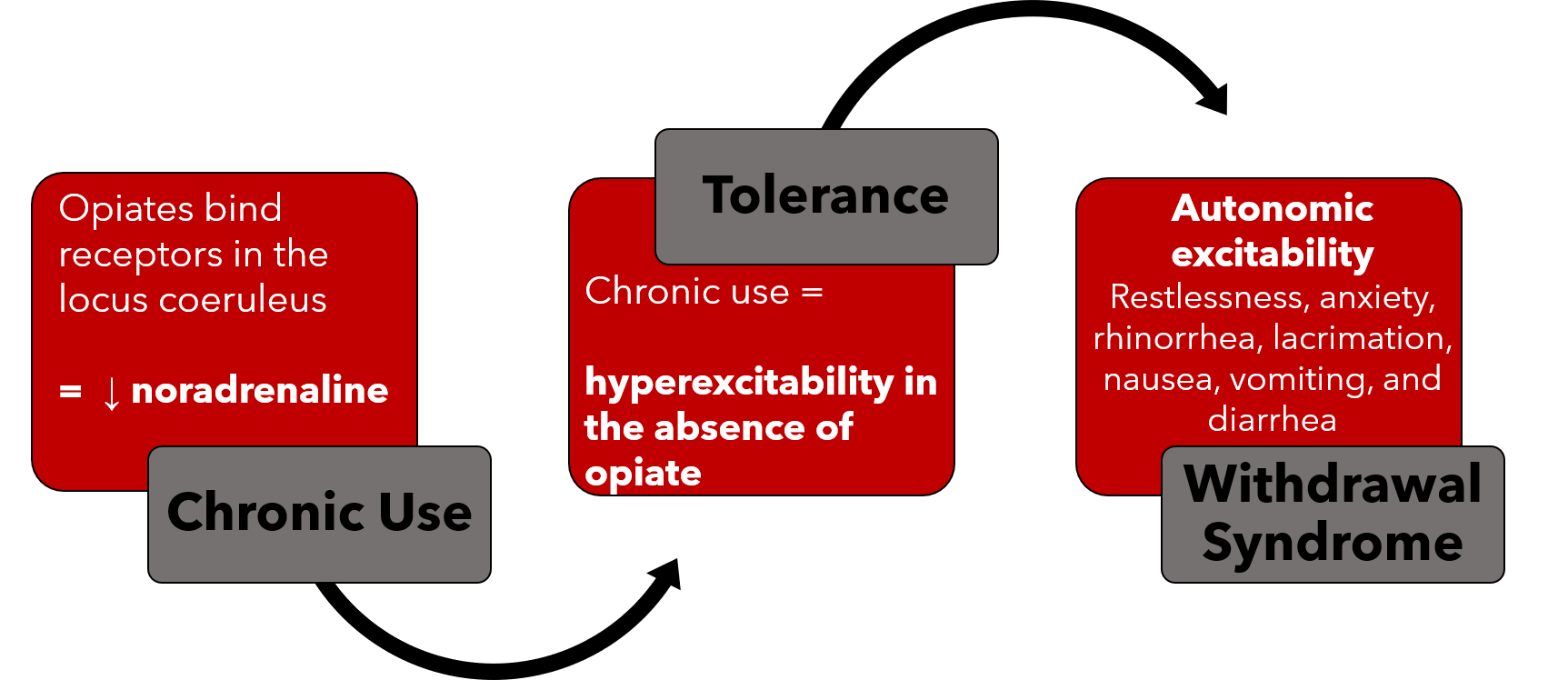
Opioid withdrawal occurs when the body becomes accustomed to the presence of opioids and struggles to function normally without them. The brain’s chemistry changes over time due to opioid use, leading to an imbalance when opioids are no longer present. This imbalance triggers a cascade of physical and psychological symptoms that can be highly uncomfortable and, in some cases, dangerous.
Symptoms of Opioid Withdrawal
The symptoms of opioid withdrawal can vary depending on factors such as the type of opioid used, the duration of use, and the individual’s overall health. These symptoms typically fall into two categories: physical and psychological.
Physical Symptoms
- Muscle aches and pains
- Nausea and vomiting
- Diarrhea
- Sweating
- Rapid heartbeat
- High blood pressure
- Dilated pupils
- Tremors or shaking
- Fever
- Runny nose and teary eyes
Psychological Symptoms
- Anxiety
- Depression
- Irritability
- Insomnia
- Difficulty concentrating
- Intense cravings for opioids
While opioid withdrawal is not typically life-threatening, it can lead to complications such as dehydration from excessive vomiting and diarrhea. In severe cases, individuals may require medical intervention to manage these symptoms safely.
The Timeline of Opioid Withdrawal
The timeline for opioid withdrawal varies depending on the specific opioid used, the method of administration, and individual factors. However, most people experience a predictable pattern of symptoms that unfold over several days to weeks.
Early Withdrawal Phase
The early phase of opioid withdrawal usually begins within six to twelve hours after the last dose of short-acting opioids, such as heroin or certain prescription painkillers. For long-acting opioids, such as methadone, symptoms may take up to thirty hours to appear. During this phase, individuals often experience:
- Mild anxiety
- Muscle aches
- Agitation
- Increased tearing
- Runny nose
Peak Withdrawal Phase
The peak phase typically occurs between one to three days after the last dose and is characterized by the most intense symptoms. This phase can include:
- Severe nausea and vomiting
- Diarrhea
- Abdominal cramping
- Sweating
- Goosebumps
- Insomnia
This stage is often the most challenging for individuals undergoing withdrawal, as the combination of physical and psychological symptoms can feel overwhelming.
Late Withdrawal Phase
After the peak phase, symptoms gradually begin to subside. Most physical symptoms resolve within five to seven days, although psychological symptoms such as anxiety, depression, and cravings can persist for weeks or even months. This extended period is sometimes referred to as post-acute withdrawal syndrome (PAWS).
Managing Opioid Withdrawal
Managing opioid withdrawal requires a comprehensive approach that addresses both the physical and psychological aspects of the process. Medical supervision and support are essential to ensure safety and increase the likelihood of successful recovery.
Medical Supervision and Detoxification
Detoxification is the process of allowing the body to rid itself of opioids while managing withdrawal symptoms. Medical detox programs provide a safe environment where individuals can receive care and support. These programs often involve:
- Medication-assisted treatment to alleviate symptoms
- Monitoring of vital signs to prevent complications
- Hydration and nutritional support
- Emotional and psychological counseling
Healthcare providers may prescribe medications such as buprenorphine, methadone, or clonidine to ease withdrawal symptoms. These medications work by reducing cravings and stabilizing the body’s response to the absence of opioids.
Behavioral Therapies and Counseling
In addition to medical interventions, behavioral therapies play a critical role in managing opioid withdrawal. Therapy helps individuals address the underlying causes of addiction, develop coping strategies, and build a support network. Common therapeutic approaches include:
- Cognitive-behavioral therapy to identify and change negative thought patterns
- Contingency management to reward positive behaviors
- Group therapy to foster peer support and accountability
- Family therapy to repair relationships and involve loved ones in the recovery process
Lifestyle Changes and Support Systems
Recovery from opioid dependence extends beyond the withdrawal phase. Making lifestyle changes and building a strong support system are essential for long-term success. Some key strategies include:
- Engaging in regular physical activity to reduce stress and improve mood
- Practicing mindfulness techniques such as meditation or yoga
- Avoiding triggers and high-risk situations
- Participating in support groups like Narcotics Anonymous
- Educating oneself about addiction and recovery
Preventing Relapse
Relapse is a common challenge during recovery from opioid dependence. To minimize the risk of relapse, individuals should:
- Continue attending therapy sessions and support group meetings
- Develop a relapse prevention plan with the help of a counselor
- Build healthy habits and routines
- Seek help immediately if cravings become overwhelming
Conclusion
Opioid withdrawal is a complex and demanding process that requires careful planning and support. By understanding the symptoms, timeline, and management strategies, individuals and their loved ones can navigate this challenging journey more effectively. With the right combination of medical care, therapy, and lifestyle changes, recovery is possible, offering hope for a healthier and more fulfilling future.