Obstetric Fistula, often abbreviated as OF, is a devastating medical condition that affects women, particularly in low-resource settings. It is characterized by an abnormal opening between the birth canal and the bladder or rectum, leading to uncontrollable leakage of urine or feces. This condition not only causes physical discomfort but also results in significant social and psychological challenges for those affected. In this article, we will explore the causes, symptoms, diagnosis, and treatment options available for Obstetric Fistula.
Causes of Obstetric Fistula
Obstetric Fistula primarily occurs due to prolonged or obstructed labor. When labor is obstructed, the pressure from the baby’s head against the mother’s pelvis can cut off blood supply to the surrounding tissues. Over time, this lack of blood flow causes the tissue to die, creating a hole or fistula between the birth canal and nearby organs such as the bladder or rectum.
Contributing Factors
- Poor Access to Healthcare: Women in remote or underserved areas often lack access to skilled medical professionals during childbirth. Without timely intervention, obstructed labor can lead to the development of a fistula.
- Early Childbearing: Girls who become pregnant at a young age are at higher risk because their bodies may not be fully developed to handle childbirth, increasing the likelihood of complications.
- Lack of Education: Limited awareness about reproductive health and family planning contributes to unintended pregnancies and unsafe deliveries.
- Poverty: Economic constraints can prevent women from seeking proper prenatal care or emergency obstetric services when needed.
Symptoms of Obstetric Fistula
The symptoms of Obstetric Fistula vary depending on the location and severity of the fistula. However, some common signs include:
Urinary Symptoms
- Continuous leakage of urine, which cannot be controlled
- Frequent urinary tract infections due to constant moisture and irritation
- Strong odor caused by the inability to maintain hygiene
Bowel Symptoms
- Involuntary passage of stool through the vagina
- Chronic skin irritation around the genital area
- Recurrent infections in the vaginal or rectal region
Psychological and Social Impact
Beyond the physical symptoms, Obstetric Fistula has profound emotional and social consequences. Women with this condition often face stigma, isolation, and depression. They may be abandoned by their families or communities due to the unpleasant smell and perceived shame associated with the condition.
Diagnosis of Obstetric Fistula
Diagnosing Obstetric Fistula requires a thorough evaluation by a healthcare professional. The process typically involves:
Medical History and Physical Examination
A detailed medical history helps identify any previous complications during childbirth. During the physical examination, the doctor checks for signs of leakage, infection, or scarring in the pelvic area.
Diagnostic Tests
- Dye Test: A harmless dye is inserted into the bladder or rectum to determine if there is leakage into the vagina.
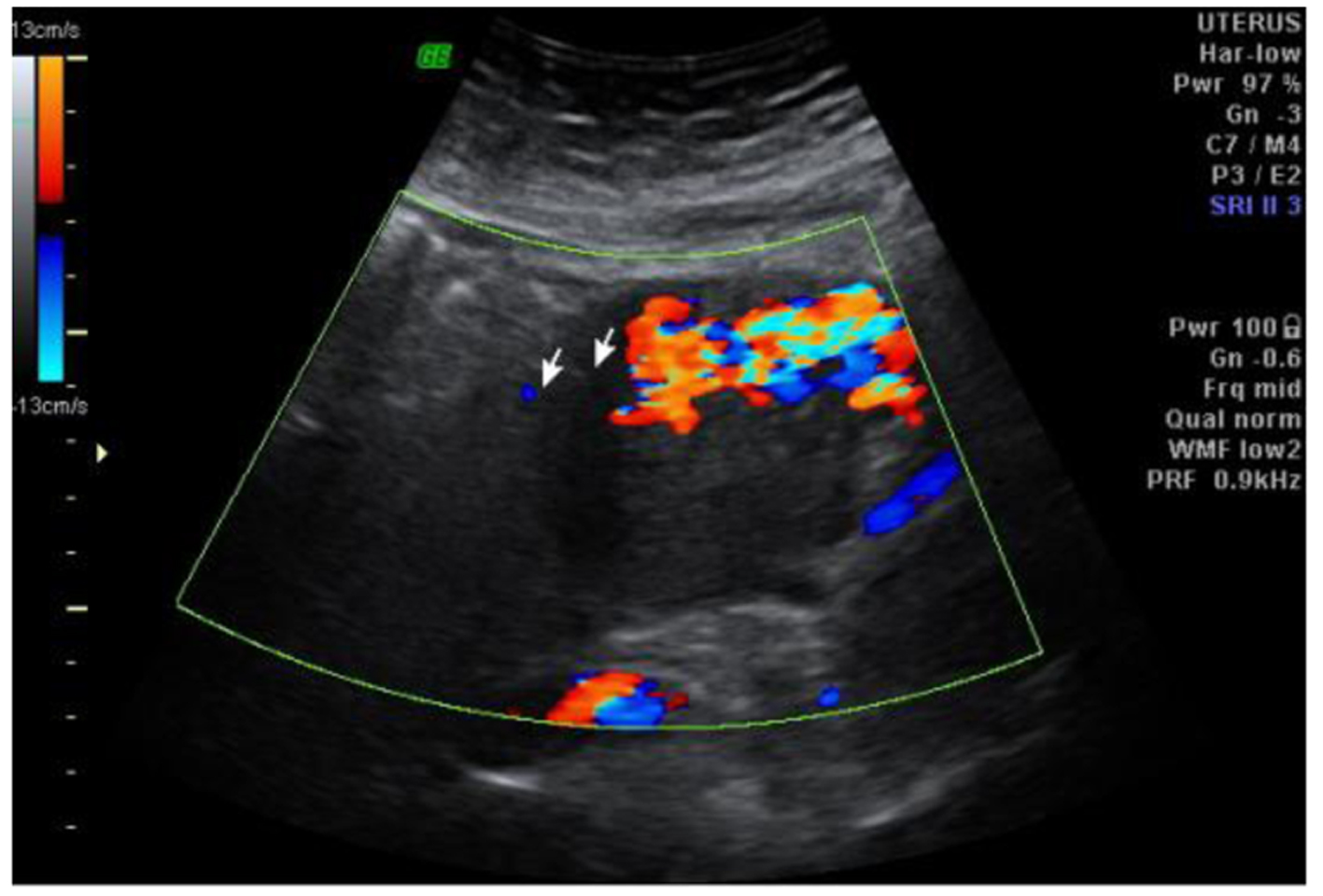
- Imaging Studies: Techniques like ultrasound, MRI, or cystoscopy may be used to locate the exact position and size of the fistula.
Referral to Specialists
In many cases, patients are referred to specialized centers where surgeons experienced in treating Obstetric Fistula can provide further assessment and care.
Treatment Options for Obstetric Fistula
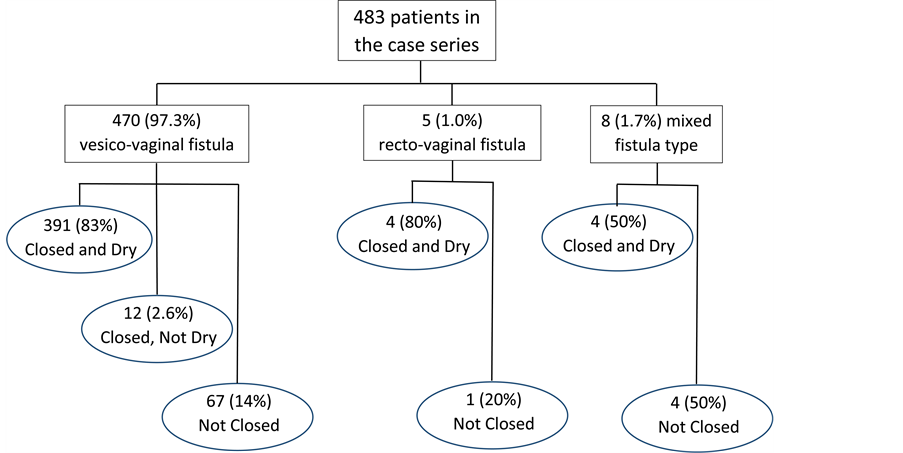
Treatment for Obstetric Fistula aims to repair the abnormal opening and restore normal function. The approach depends on the type, size, and location of the fistula, as well as the overall health of the patient.
Surgical Repair
Surgery is the most effective method for treating Obstetric Fistula. Skilled surgeons perform reconstructive procedures to close the fistula and reconnect the damaged tissues. Key aspects of surgical repair include:
- Timing: Surgery is usually performed after inflammation and infection have been treated.
- Technique: Different techniques are employed based on the complexity of the fistula. Simple fistulas may require straightforward closure, while complex cases might involve more advanced procedures.
- Postoperative Care: Patients need careful monitoring and follow-up to ensure proper healing and prevent recurrence.
Non-Surgical Interventions
In certain situations, non-surgical treatments may be considered:
- Catheterization: For small fistulas, inserting a catheter to drain urine or stool may allow the tissues to heal naturally over time.
- Medications: Antibiotics are prescribed to manage infections before or after surgery.
Rehabilitation and Support
Addressing the broader impact of Obstetric Fistula is crucial for recovery. Rehabilitation programs focus on:
- Physical Therapy: Exercises to strengthen pelvic muscles and improve mobility.
- Counseling: Psychological support to help women cope with trauma, rebuild self-esteem, and reintegrate into society.
- Vocational Training: Empowering women with skills to regain independence and financial stability.
Prevention Strategies
Preventing Obstetric Fistula requires addressing its root causes and improving maternal healthcare systems. Some strategies include:
Improving Access to Prenatal and Delivery Services
- Ensuring that all women have access to skilled birth attendants and emergency obstetric care.
- Establishing transportation networks to facilitate timely access to hospitals during labor.
Promoting Education and Awareness
- Educating communities about safe pregnancy practices and the importance of seeking medical assistance during childbirth.
- Raising awareness about family planning methods to reduce unintended pregnancies.
Empowering Women
- Providing economic opportunities and education to empower women and delay early marriages.
- Encouraging gender equality to reduce societal barriers that limit women’s access to healthcare.
Global Efforts to Combat Obstetric Fistula
International organizations, governments, and non-profits are working together to eliminate Obstetric Fistula worldwide. Initiatives include:
- Training Programs: Equipping healthcare workers with the skills to diagnose and treat Obstetric Fistula effectively.
- Free Surgeries: Offering free or subsidized surgical repairs to women in need.
- Advocacy Campaigns: Raising global awareness and advocating for policy changes to prioritize maternal health.