Neuralgia, commonly referred to as nerve pain, is a condition characterized by sharp, burning, or throbbing pain caused by damage or irritation to the nerves. This type of pain can significantly affect a person’s quality of life, making even simple daily activities challenging. Understanding the different types, causes, symptoms, and treatment options for this condition is crucial for effective management and relief. In this article, we will delve into the various aspects of nerve pain, shedding light on what it entails and how it can be addressed.
What is Nerve Pain?
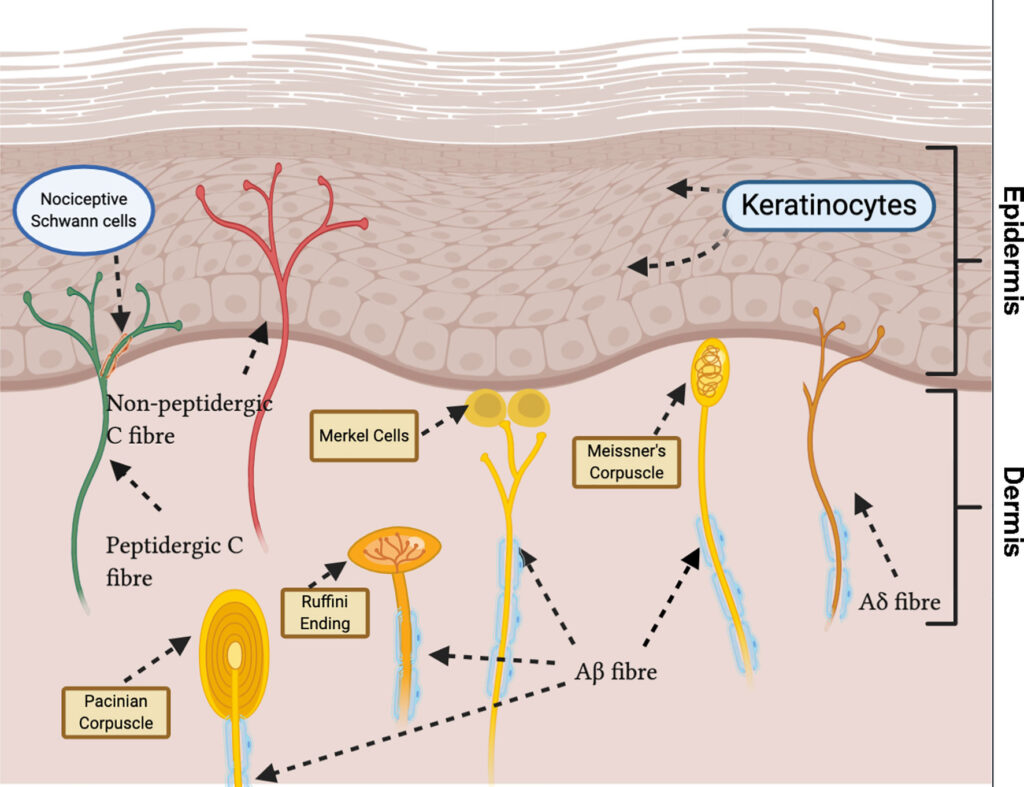
Nerve pain occurs when there is damage or dysfunction in the nervous system. Unlike other types of pain that arise from injuries to muscles, bones, or tissues, nerve pain originates directly from the nerves themselves. The pain can manifest in various forms, including sharp, stabbing sensations, burning feelings, or electric shock-like episodes. It may also be accompanied by tingling, numbness, or hypersensitivity to touch.
How Nerve Pain Differs from Other Types of Pain
- Origin: Nerve pain stems from issues within the nervous system, while other types of pain are typically caused by external factors like injuries or inflammation.
- Sensation: The pain is often described as unusual or intense, differing from the dull ache or soreness associated with muscle or joint pain.
- Duration: Nerve pain can persist long after the initial injury or condition has healed, making it chronic in many cases.
Types of Nerve Pain
There are several types of nerve pain, each with distinct characteristics and affected areas. Below are some of the most common types:
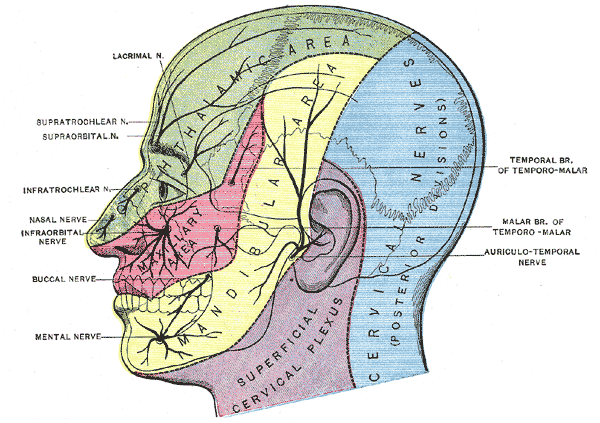
Trigeminal Neuralgia
Trigeminal neuralgia affects the trigeminal nerve, which is responsible for transmitting sensations from the face to the brain. This condition is known for causing sudden, severe, and electric shock-like pain in the face. Even mild stimuli, such as brushing teeth or applying makeup, can trigger episodes of pain.
Postherpetic Neuralgia
This type of nerve pain occurs as a complication of shingles, a viral infection caused by the varicella-zoster virus. After the rash and blisters from shingles heal, some individuals continue to experience persistent pain in the affected area. This lingering discomfort is known as postherpetic neuralgia.
Diabetic Neuropathy
Diabetic neuropathy is a form of nerve damage that arises as a complication of diabetes. High blood sugar levels over time can injure nerves throughout the body, but the legs and feet are most commonly affected. Symptoms include numbness, tingling, and sharp pain.
Occipital Neuralgia
Occipital neuralgia involves irritation or injury to the occipital nerves, which run from the base of the neck to the scalp. This condition often leads to headaches characterized by piercing, throbbing, or electric shock-like pain in the upper neck, back of the head, or behind the ears.
Peripheral Neuropathy
Peripheral neuropathy refers to damage to the peripheral nerves, which connect the brain and spinal cord to the rest of the body. This condition can result from various causes, including infections, autoimmune diseases, and exposure to toxins. Symptoms include weakness, numbness, and pain, usually in the hands and feet.
Causes of Nerve Pain
The underlying causes of nerve pain can vary widely, ranging from medical conditions to external factors. Below are some of the most common causes:
Injury or Trauma
Physical injuries, such as those sustained in accidents or surgeries, can damage nerves and lead to nerve pain. For example, a herniated disc in the spine can compress nearby nerves, causing radiating pain down the arms or legs.
Infections
Certain infections can attack the nervous system and cause nerve pain. Shingles, Lyme disease, and HIV are examples of infections that may lead to nerve-related symptoms.
Chronic Diseases
Conditions like diabetes, multiple sclerosis, and cancer can contribute to nerve pain. Diabetes, in particular, is a leading cause of nerve damage due to prolonged high blood sugar levels.
Toxins and Medications
Exposure to certain chemicals, heavy metals, or medications can harm the nerves. Chemotherapy drugs, for instance, are known to cause peripheral neuropathy as a side effect.
Compression or Entrapment
Nerves can become compressed or entrapped due to repetitive motions, poor posture, or structural abnormalities. Carpal tunnel syndrome, for example, occurs when the median nerve in the wrist is compressed, leading to pain, numbness, and weakness in the hand.
Symptoms of Nerve Pain
The symptoms of nerve pain can vary depending on the type and location of the affected nerves. However, some common signs and symptoms include:
- Sharp, shooting, or stabbing pain
- Burning or tingling sensations
- Numbness or loss of sensation
- Hypersensitivity to touch or temperature
- Muscle weakness or paralysis
- Electric shock-like sensations
When to Seek Medical Attention
If you experience persistent or worsening nerve pain, it is important to consult a healthcare professional. Early diagnosis and treatment can help prevent further nerve damage and improve outcomes. Additionally, seek immediate medical attention if the pain is accompanied by symptoms such as fever, unexplained weight loss, or difficulty moving.
Treatment Options for Nerve Pain
Managing nerve pain often requires a combination of approaches tailored to the individual’s specific condition and needs. Below are some of the most common treatment options:
Medications
Several medications can help alleviate nerve pain. These include:
- Pain Relievers: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may provide temporary relief for mild cases.
- Anticonvulsants: Medications originally developed to treat epilepsy, such as gabapentin and pregabalin, are often prescribed for nerve pain.
- Antidepressants: Certain antidepressants, such as amitriptyline and duloxetine, can help reduce nerve pain by altering the way the brain processes pain signals.
- Topical Treatments: Creams, gels, or patches containing lidocaine or capsaicin can be applied directly to the affected area for localized relief.
Physical Therapy
Physical therapy can play a crucial role in managing nerve pain, particularly when it is caused by compression or injury. A physical therapist can design a personalized exercise program to strengthen muscles, improve flexibility, and reduce pressure on the nerves.
Nerve Blocks
Nerve blocks involve injecting anesthetic or anti-inflammatory medications near the affected nerve to temporarily block pain signals. This procedure can provide significant relief for certain types of nerve pain, such as occipital neuralgia.
Lifestyle Modifications
Making lifestyle changes can also help manage nerve pain. These include:
- Maintaining a healthy diet to support nerve health
- Engaging in regular exercise to improve circulation and reduce stress
- Avoiding alcohol and tobacco, which can exacerbate nerve damage
- Practicing relaxation techniques, such as meditation or yoga, to cope with chronic pain
Surgical Interventions
In severe cases where conservative treatments fail, surgery may be considered. Procedures such as decompression surgery or nerve repair can address underlying structural issues causing nerve pain.
Alternative Therapies
Some individuals find relief through alternative therapies, such as acupuncture, chiropractic care, or biofeedback. While these methods may not work for everyone, they can be worth exploring as part of a comprehensive treatment plan.