Inflammation of muscles, commonly referred to as Myositis, is a condition that affects the muscular system, leading to pain, weakness, and swelling. While the exact cause of this condition may vary, it often stems from autoimmune disorders or infections. Understanding the causes, symptoms, and treatment options for muscle inflammation is crucial for early diagnosis and effective management. This article delves into the details of muscle inflammation, offering insights into its origins, signs to watch for, and available treatments.
What Is Muscle Inflammation?
Muscle inflammation occurs when the body’s immune system mistakenly targets healthy muscle tissues, causing them to become inflamed. This condition can affect people of all ages, though certain types are more prevalent in specific age groups. The inflammation can lead to discomfort, restricted movement, and even permanent damage if left untreated. Muscle inflammation is not a single disease but rather a group of conditions that share similar symptoms and underlying mechanisms.
Types of Muscle Inflammation
- Polymyositis: A condition that causes muscle weakness, typically affecting muscles closest to the trunk of the body.
- Dermatomyositis: Similar to polymyositis but accompanied by a distinctive skin rash.
- Inclusion Body Myositis: A progressive disorder that primarily affects older adults and leads to gradual muscle weakening.
- Toxic Myositis: Caused by exposure to certain medications, drugs, or toxins.
- Infectious Myositis: Triggered by bacterial, viral, or parasitic infections.
Causes of Muscle Inflammation
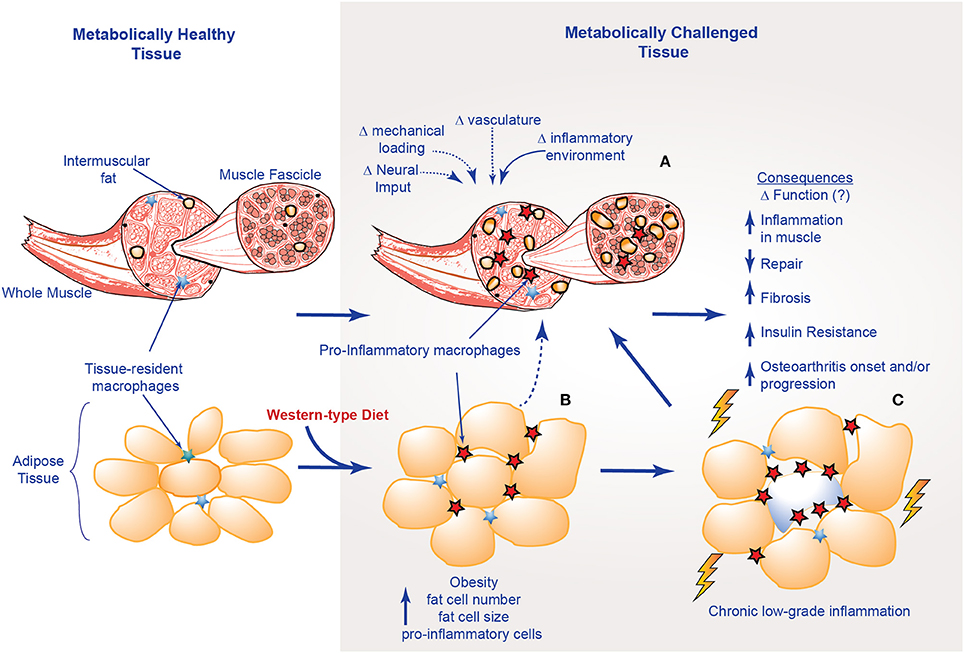
The exact cause of muscle inflammation can vary depending on the type of condition. However, most cases are linked to autoimmune responses, infections, or external factors such as medications or injuries.
Autoimmune Disorders
In autoimmune-related muscle inflammation, the immune system mistakenly attacks healthy muscle tissues. This can happen due to genetic predisposition or environmental triggers. For example, polymyositis and dermatomyositis are believed to result from an overactive immune response that damages muscle fibers.
Infections
Certain infections can also lead to muscle inflammation. Viral infections like influenza or the human immunodeficiency virus can trigger an inflammatory response in the muscles. Bacterial infections, such as those caused by staphylococcus or streptococcus, may also result in localized or systemic muscle inflammation.
Medications and Toxins
Some medications, including statins used to lower cholesterol, have been associated with muscle inflammation as a side effect. Similarly, exposure to toxins like alcohol, cocaine, or heavy metals can irritate muscle tissues and lead to inflammation.
Trauma and Overuse
Physical trauma or repetitive strain can cause acute muscle inflammation. Athletes or individuals who engage in strenuous physical activity without proper rest may experience muscle soreness and swelling due to micro-tears in the muscle fibers.
Symptoms of Muscle Inflammation
The symptoms of muscle inflammation can vary depending on the underlying cause and the severity of the condition. However, there are some common signs that individuals should be aware of.
Muscle Weakness
One of the hallmark symptoms of muscle inflammation is muscle weakness. This often affects the muscles closest to the body’s core, such as those in the shoulders, hips, and thighs. Individuals may find it difficult to lift objects, climb stairs, or even stand up from a seated position.
Muscle Pain and Tenderness
Pain and tenderness in the affected muscles are common symptoms. The pain may range from mild discomfort to severe, debilitating aches. Some individuals may also experience muscle stiffness, particularly after periods of inactivity.
Fatigue
Chronic fatigue is another frequent symptom of muscle inflammation. The constant immune response and muscle damage can leave individuals feeling exhausted, even after minimal physical exertion.
Skin Rashes
In cases of dermatomyositis, a reddish or purplish rash may appear on the face, knuckles, elbows, knees, or chest. This rash often precedes muscle weakness and can serve as an early warning sign of the condition.
Difficulty Swallowing
Swallowing difficulties, also known as dysphagia, can occur in severe cases of muscle inflammation. This happens when the muscles involved in swallowing become weakened or inflamed.
Joint Pain
Some individuals with muscle inflammation may also experience joint pain and swelling. This is particularly common in autoimmune-related conditions like polymyositis and dermatomyositis.
Diagnosis of Muscle Inflammation
Diagnosing muscle inflammation requires a combination of clinical evaluation, laboratory tests, and imaging studies. Early and accurate diagnosis is essential for effective treatment.
Clinical Evaluation
A healthcare provider will begin by taking a detailed medical history and conducting a physical examination. They will assess muscle strength, range of motion, and any visible signs of inflammation, such as rashes or swelling.
Blood Tests
Blood tests can help identify markers of inflammation, such as elevated levels of creatine kinase, an enzyme released when muscle tissue is damaged. Other blood tests may check for autoimmune antibodies that are often present in conditions like polymyositis or dermatomyositis.
Electromyography
This test involves inserting small needles into the muscles to measure their electrical activity. Abnormal patterns can indicate muscle inflammation or damage.
Muscle Biopsy
In some cases, a small sample of muscle tissue may be removed and examined under a microscope. This can provide definitive evidence of inflammation and help differentiate between various types of muscle disorders.
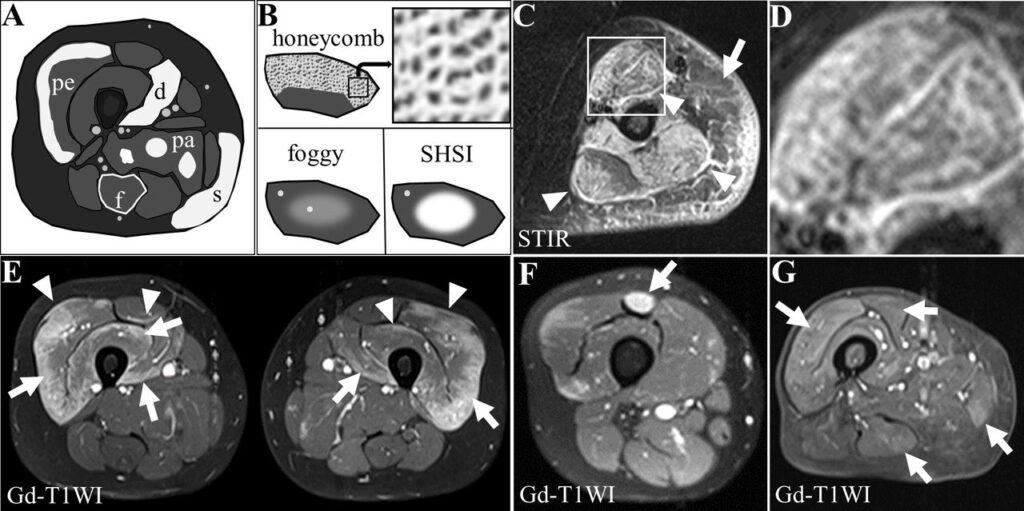
Imaging Studies
Magnetic resonance imaging or ultrasound may be used to visualize muscle tissues and identify areas of inflammation or damage.
Treatment Options for Muscle Inflammation
While there is no cure for many forms of muscle inflammation, several treatment options can help manage symptoms and improve quality of life.
Medications
Medications are often the first line of treatment for muscle inflammation. These may include:
- Corticosteroids: These powerful anti-inflammatory drugs can reduce swelling and suppress the immune system’s response.
- Immunosuppressants: Medications like methotrexate or azathioprine may be prescribed to control the immune system in autoimmune-related conditions.
- Pain Relievers: Over-the-counter or prescription pain medications can help alleviate discomfort.
Physical Therapy
Physical therapy plays a crucial role in managing muscle inflammation. A tailored exercise program can help maintain muscle strength, flexibility, and function. Therapists may also use techniques like massage or heat therapy to reduce pain and stiffness.
Lifestyle Modifications
Making certain lifestyle changes can complement medical treatments and improve overall well-being:
- Balanced Diet: Consuming a nutrient-rich diet can support muscle health and boost the immune system.
- Adequate Rest: Ensuring sufficient rest and avoiding overexertion can prevent further muscle damage.
- Stress Management: Techniques like meditation or yoga can help reduce stress, which may exacerbate symptoms.
Alternative Therapies
Some individuals may find relief through alternative therapies such as acupuncture, herbal supplements, or chiropractic care. However, these should always be discussed with a healthcare provider to ensure safety and efficacy.
Living with Muscle Inflammation
Managing muscle inflammation often requires a multidisciplinary approach involving healthcare providers, physical therapists, and nutritionists. By staying informed and proactive, individuals can take steps to minimize symptoms and maintain their quality of life.
Support Groups
Joining a support group can provide emotional support and practical advice for individuals living with muscle inflammation. Sharing experiences with others who understand the challenges of the condition can be incredibly empowering.
Regular Monitoring
Regular follow-up appointments with healthcare providers are essential to monitor the progression of the condition and adjust treatment plans as needed.