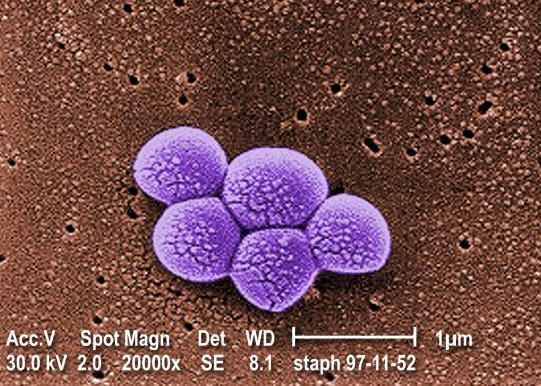
Methicillin-resistant Staphylococcus aureus, commonly known as MRSA, is a type of bacterial infection that has become a significant concern in healthcare settings and communities worldwide. This infection is caused by a strain of bacteria that has developed resistance to many antibiotics, making it challenging to treat. Understanding what this infection is, its causes, symptoms, and available treatments is crucial for preventing its spread and ensuring timely medical intervention.
What is Methicillin-resistant Staphylococcus aureus?
Methicillin-resistant Staphylococcus aureus refers to a specific type of bacteria that is resistant to several antibiotics, including methicillin, which was once a standard treatment for staph infections. Staphylococcus aureus is a common bacterium found on the skin or in the noses of healthy individuals. While most strains of this bacterium are harmless, some can cause infections, ranging from minor skin issues to life-threatening conditions like pneumonia or bloodstream infections.
The resistant nature of this particular strain makes it especially dangerous because it limits the options for effective treatment. When left untreated or improperly managed, infections caused by this bacterium can lead to severe complications, prolonged hospital stays, and increased healthcare costs.
Causes of Methicillin-resistant Staphylococcus aureus Infections
Several factors contribute to the development and spread of these infections. Below are the primary causes:
1. Antibiotic Overuse and Misuse
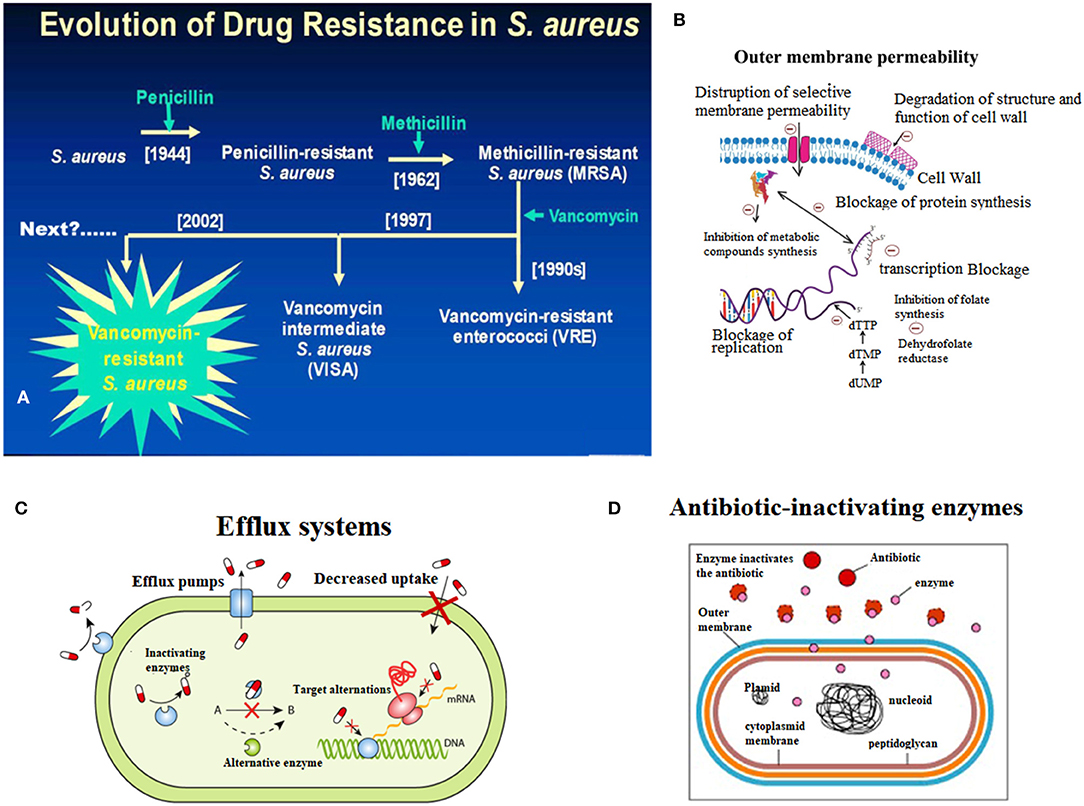
- Overprescription of antibiotics has led to the emergence of resistant bacterial strains. When antibiotics are used unnecessarily or incorrectly, bacteria have the opportunity to adapt and develop resistance mechanisms.
- Incomplete antibiotic courses also play a role. If a patient stops taking antibiotics before finishing the prescribed course, surviving bacteria can multiply and evolve into resistant forms.
2. Close Contact with Infected Individuals
- This infection often spreads through direct contact with an infected person or contaminated surfaces. Skin-to-skin contact, sharing personal items like towels or razors, and poor hygiene practices increase the risk of transmission.
- Crowded environments such as hospitals, nursing homes, schools, and gyms provide ideal conditions for the bacteria to spread.
3. Weakened Immune System
- Individuals with weakened immune systems, such as those undergoing chemotherapy, living with chronic illnesses, or recovering from surgery, are more susceptible to these infections.
- Medical devices like catheters or ventilators can also serve as entry points for bacteria, increasing the likelihood of infection.
Symptoms of Methicillin-resistant Staphylococcus aureus Infections
The symptoms of these infections vary depending on the location and severity of the infection. Some common signs include:
1. Skin Infections
- Boils or abscesses: Painful red bumps filled with pus that may resemble spider bites.
- Cellulitis: A swollen, red area of skin that feels warm and tender to the touch.
- Impetigo: Red sores that break open, ooze fluid, and develop a yellow-brown crust.
2. Wound Infections
- Infected surgical wounds may appear red, swollen, and discharge pus or other fluids.
- Pain around the wound site and fever are additional indicators of an infection.
3. Severe Infections
- Pneumonia: Symptoms include shortness of breath, chest pain, coughing, and high fever.
- Bloodstream infections: These can cause sepsis, a life-threatening condition characterized by rapid heart rate, confusion, extreme fatigue, and low blood pressure.
If you notice any of these symptoms, especially after recent hospitalization or exposure to high-risk environments, seek medical attention immediately.
Treatment Options for Methicillin-resistant Staphylococcus aureus Infections
Treating these infections requires a careful approach due to their resistance to many antibiotics. Below are the primary treatment methods used:
1. Antibiotics
- Although resistant to many drugs, certain antibiotics remain effective against these infections. Vancomycin, daptomycin, and linezolid are examples of medications commonly prescribed.
- Doctors may perform tests to determine which antibiotic will work best for a specific case. This process, known as susceptibility testing, helps ensure targeted and effective treatment.
2. Drainage Procedures
- For skin infections like boils or abscesses, doctors may need to drain the pus to relieve pain and promote healing.
- This procedure is typically performed under sterile conditions to prevent further contamination.
3. Surgical Intervention
- In severe cases, such as when the infection affects internal organs or deep tissues, surgery may be necessary to remove damaged tissue or infected areas.
- For example, if an artificial joint becomes infected, it might need to be replaced entirely.
4. Supportive Care
- Patients with severe infections may require supportive care, such as intravenous fluids, oxygen therapy, or medications to stabilize blood pressure.
- Hospitalization is often necessary for monitoring and managing complications.
Prevention Strategies
Preventing the spread of these infections involves adopting good hygiene practices and minimizing unnecessary antibiotic use. Here are some effective prevention strategies:
1. Hand Hygiene
- Regular handwashing with soap and water is one of the simplest yet most effective ways to prevent the spread of bacteria.
- Use alcohol-based hand sanitizers when soap and water are not available.
2. Proper Wound Care
- Cover cuts, scrapes, and wounds with clean bandages until they heal completely.
- Avoid sharing personal items like razors, towels, or clothing, as these can harbor bacteria.
3. Safe Practices in Healthcare Settings
- Hospitals and clinics should adhere to strict infection control protocols, including regular disinfection of equipment and surfaces.
- Healthcare workers must practice proper hand hygiene and wear protective gear when interacting with patients.
4. Educating the Public
- Raising awareness about the dangers of antibiotic misuse and the importance of completing prescribed courses can help combat the rise of resistant bacteria.
- Community programs aimed at promoting hygiene and safe behaviors can reduce the incidence of these infections outside healthcare facilities.
Living with Methicillin-resistant Staphylococcus aureus
Some individuals may carry this bacterium without showing any symptoms, a condition known as colonization. While colonization does not necessarily lead to illness, carriers can still transmit the bacteria to others. To minimize risks:
- Practice good hygiene consistently.
- Inform healthcare providers about your carrier status before undergoing medical procedures.
- Follow guidelines provided by healthcare professionals to prevent spreading the bacteria to family members or close contacts.
Emerging Research and Innovations
Scientists and researchers are actively working to address the challenges posed by these infections. Recent advancements include:
- Development of new antibiotics designed to target resistant strains.
- Exploration of alternative therapies, such as phage therapy, which uses viruses to attack bacteria.
- Improved diagnostic tools to identify infections quickly and accurately.
These innovations offer hope for better management and eventual control of these difficult-to-treat infections.