Meralgia Paresthetica, also known as Lateral Femoral Cutaneous Neuropathy or Meralgia Paresthetica Syndrome, is a condition that causes numbness, tingling, and burning pain in the outer thigh. This condition occurs when the lateral femoral cutaneous nerve, which supplies sensation to the surface of your thigh, is compressed or irritated. It is a relatively common yet often underdiagnosed issue that can significantly affect an individual’s quality of life. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition.

Understanding the Anatomy
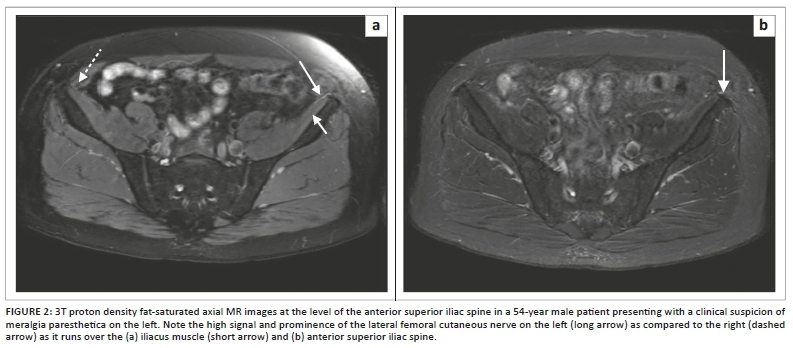
To fully grasp the nature of this condition, it is essential to understand the anatomy of the lateral femoral cutaneous nerve. This nerve originates from the lumbar plexus, specifically from the second and third lumbar nerve roots. It travels through the pelvis and exits near the anterior superior iliac spine, which is the bony prominence at the front of the hip. From there, it runs beneath the inguinal ligament and supplies sensation to the skin on the outer thigh.
The lateral femoral cutaneous nerve is purely sensory, meaning it does not control any muscles. Its sole function is to provide sensation to the surface of the thigh. When this nerve becomes compressed or irritated, it leads to abnormal sensations such as numbness, tingling, or burning pain in the area it serves.
Common Causes of Nerve Compression
Several factors can contribute to the compression or irritation of the lateral femoral cutaneous nerve. Below are some of the most common causes:
Tight Clothing
- Wearing tight belts, corsets, or pants can put pressure on the nerve as it passes beneath the inguinal ligament.
- Occupations or activities that require wearing heavy tool belts around the waist can also compress the nerve.
Obesity
- Excess weight can increase pressure on the nerve, particularly in the abdominal and pelvic regions.
- Abdominal fat can push down on the nerve as it exits the pelvis, leading to irritation.
Pregnancy
- The growing uterus during pregnancy can exert additional pressure on the nerve.
- Hormonal changes during pregnancy may also contribute to ligament laxity, further affecting nerve function.
Trauma or Injury
- Direct trauma to the hip or thigh region can damage the nerve.
- Surgical procedures in the pelvic or abdominal area may inadvertently affect the nerve.
Prolonged Postures
- Sitting or standing for extended periods, especially with poor posture, can compress the nerve.
- Crossing the legs frequently may also contribute to nerve irritation.
Symptoms of the Condition
The hallmark symptoms of this condition include numbness, tingling, and burning pain in the outer thigh. These symptoms are typically confined to the area supplied by the lateral femoral cutaneous nerve and do not extend beyond the knee. Below is a detailed breakdown of the symptoms:
Numbness
Patients often describe a loss of sensation or a “pins and needles” feeling in the outer thigh. This numbness may come and go or persist for extended periods.
Burning Pain
A characteristic symptom is a sharp, burning pain that feels like it is on the surface of the skin. The pain is usually more pronounced when standing or walking and may improve when sitting or lying down.
Tingling Sensations
Tingling or a “prickly” feeling is another common complaint. Some patients describe it as similar to the sensation experienced when a limb “falls asleep.”
Hypersensitivity
In some cases, the affected area may become hypersensitive to touch or pressure. Even light contact, such as clothing brushing against the thigh, can cause discomfort.
Diagnosing the Condition
Diagnosing this condition can be challenging because its symptoms overlap with other conditions, such as sciatica or nerve root compression in the lower back. However, a thorough evaluation by a healthcare professional can help identify the underlying cause. Below are the steps involved in diagnosing the condition:
Medical History
The doctor will begin by taking a detailed medical history. They will ask about the onset, duration, and nature of the symptoms, as well as any potential contributing factors such as tight clothing, obesity, or recent injuries.
Physical Examination
A physical examination is crucial for identifying signs of nerve compression. The doctor may perform specific tests, such as applying pressure over the inguinal ligament or asking the patient to assume certain postures, to reproduce the symptoms.
Diagnostic Tests
In some cases, imaging studies or nerve conduction tests may be necessary to rule out other conditions or confirm the diagnosis:
- X-rays or MRI: These imaging studies can help identify structural abnormalities, such as bone spurs or tumors, that may be compressing the nerve.
- Nerve Conduction Studies: These tests measure the speed and strength of electrical signals traveling through the nerve, helping to assess its function.
Treatment Options
Treatment for this condition focuses on relieving nerve compression and managing symptoms. In most cases, conservative measures are effective, but more severe cases may require medical intervention. Below are the primary treatment options:
Lifestyle Modifications
Making simple changes to daily habits can often alleviate symptoms:
- Loose Clothing: Avoid wearing tight belts, corsets, or pants that put pressure on the waist or groin area.
- Weight Management: Losing excess weight can reduce pressure on the nerve.
- Ergonomic Adjustments: Modify workstations or seating arrangements to maintain proper posture.
Medications
Over-the-counter or prescription medications can help manage pain and inflammation:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen or naproxen can reduce inflammation and relieve pain.
- Topical Treatments: Creams or patches containing lidocaine or capsaicin may provide localized relief.
Physical Therapy
Physical therapy can strengthen the surrounding muscles and improve flexibility, reducing pressure on the nerve:
- Stretching Exercises: Gentle stretches targeting the hip and thigh can alleviate tension.
- Postural Training: Learning how to sit, stand, and move correctly can prevent further irritation.
Injections
In cases where conservative treatments are ineffective, corticosteroid injections may be recommended:
- Anti-Inflammatory Injections: These injections can reduce inflammation around the nerve and provide temporary relief.
Surgical Intervention
Surgery is rarely required but may be considered if symptoms are severe and persistent:
- Nerve Decompression Surgery: This procedure involves releasing the nerve from surrounding tissues that are causing compression.
Preventing Recurrence
While this condition is often manageable with treatment, taking preventive measures can reduce the risk of recurrence:
- Maintain a Healthy Weight: Keeping body weight within a healthy range reduces pressure on the nerve.
- Choose Comfortable Clothing: Opt for loose-fitting garments that do not constrict the waist or groin area.
- Practice Good Posture: Be mindful of posture while sitting, standing, and walking to avoid unnecessary strain.
By understanding the causes, symptoms, and treatment options for this condition, individuals can take proactive steps to manage their symptoms and improve their quality of life.