Lynch Syndrome, also known as Hereditary Nonpolyposis Colorectal Cancer (HNPCC), is a genetic condition that significantly increases the risk of developing various types of cancer. This syndrome is caused by mutations in specific genes responsible for repairing errors in DNA replication. Individuals with Lynch Syndrome face a higher likelihood of being diagnosed with cancers such as colorectal, endometrial, ovarian, and others. Understanding this condition is crucial for early detection, prevention, and management of associated risks.
What is Lynch Syndrome?
Lynch Syndrome is an inherited disorder that predisposes individuals to a variety of cancers. It occurs when there are mutations in certain genes that play a vital role in maintaining the integrity of DNA. These genes are part of a system known as the mismatch repair system, which corrects mistakes that occur during DNA replication. When these genes are defective, errors accumulate in the DNA, leading to uncontrolled cell growth and, eventually, cancer.
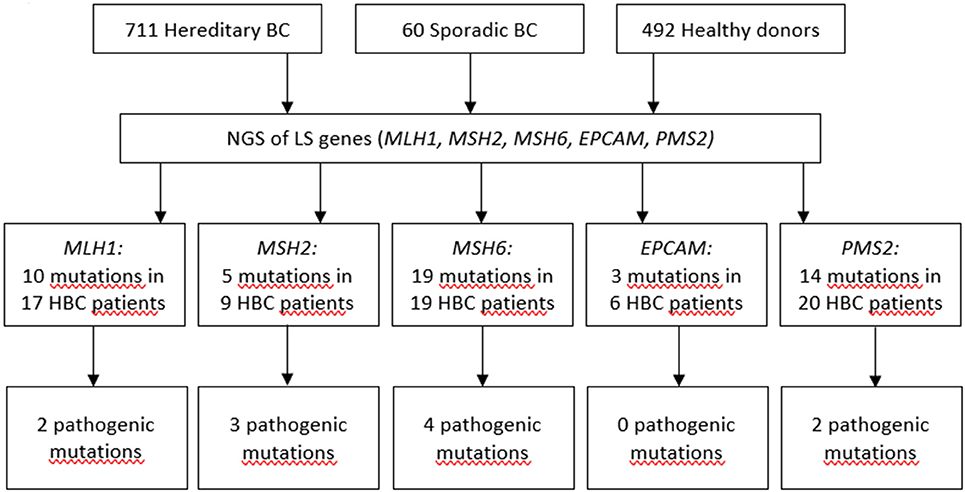
The most commonly affected genes in this syndrome include MLH1, MSH2, MSH6, PMS2, and EPCAM. Mutations in any of these genes can impair the body’s ability to repair DNA errors, increasing the likelihood of cancer development.
How Does Lynch Syndrome Increase Cancer Risk?
The mismatch repair system acts as a proofreading mechanism for DNA. When this system is compromised due to mutations, errors in the DNA sequence are not corrected. Over time, these errors accumulate and lead to changes in genes that control cell growth and division. Such changes can result in the formation of tumors.
Cancers associated with Lynch Syndrome tend to develop at an earlier age compared to sporadic cancers. Additionally, individuals with this condition often have a family history of cancer, particularly colorectal and endometrial cancers. The risk varies depending on the specific gene mutation involved, but it is generally much higher than in the general population.
Types of Cancers Linked to Lynch Syndrome
- Colorectal Cancer: This is the most common cancer associated with Lynch Syndrome. Individuals with this condition have a lifetime risk of developing colorectal cancer that can exceed 80 percent.
- Endometrial Cancer: Women with Lynch Syndrome are at a significantly increased risk of developing cancer of the lining of the uterus, with risks ranging from 40 to 60 percent.
- Ovarian Cancer: The risk of ovarian cancer in women with Lynch Syndrome is approximately 10 to 15 percent, which is higher than the general population.
- Other Cancers: Lynch Syndrome also increases the risk of cancers of the stomach, small intestine, liver, gallbladder ducts, urinary tract, brain, and skin.
Diagnosing Lynch Syndrome
Identifying Lynch Syndrome involves a combination of clinical evaluation, family history assessment, and genetic testing. Early diagnosis is critical because it allows individuals to take preventive measures and undergo regular screenings to detect cancer at an early stage.
Family History Assessment
A detailed family history is often the first step in diagnosing this condition. Healthcare providers look for patterns of cancer within families, especially if multiple relatives have been diagnosed with colorectal or endometrial cancer at a young age. A strong family history of these cancers may prompt further investigation.
Genetic Testing
Genetic testing is the definitive method for diagnosing Lynch Syndrome. It involves analyzing a blood or saliva sample to identify mutations in the genes associated with the condition. If a mutation is found, it confirms the diagnosis, and other family members may also be tested to determine their risk.
Tumor Testing
In some cases, tumor testing is performed before genetic testing. This involves examining cancerous tissue for signs of mismatch repair deficiency or microsatellite instability, which are hallmarks of Lynch Syndrome. If these signs are present, it suggests the need for genetic testing.
Managing the Risks Associated with Lynch Syndrome
Once diagnosed, individuals with Lynch Syndrome can take steps to manage their increased cancer risk. These strategies focus on early detection, prevention, and lifestyle modifications.
Regular Screenings
Frequent screenings are essential for individuals with Lynch Syndrome. Colonoscopies are recommended every one to two years starting at age 20 to 25, or earlier if there is a family history of early-onset colorectal cancer. For women, regular screenings for endometrial and ovarian cancers, such as transvaginal ultrasounds and endometrial biopsies, are also important.
Prophylactic Surgeries
In some cases, prophylactic surgeries may be considered to reduce cancer risk. For example, women with Lynch Syndrome may choose to undergo a hysterectomy or removal of the ovaries to prevent endometrial and ovarian cancers. Similarly, individuals at high risk for colorectal cancer may consider colectomy, a surgical procedure to remove part or all of the colon.
Lifestyle Modifications
Adopting a healthy lifestyle can also help mitigate cancer risk. This includes maintaining a balanced diet rich in fruits, vegetables, and whole grains, exercising regularly, avoiding tobacco, and limiting alcohol consumption. These measures not only reduce cancer risk but also improve overall health.
Medications for Risk Reduction
Some studies suggest that medications like aspirin may help lower the risk of colorectal cancer in individuals with Lynch Syndrome. However, the use of such medications should be discussed with a healthcare provider, as they may have side effects or interact with other treatments.
Raising Awareness and Supporting Families
Raising awareness about Lynch Syndrome is crucial for ensuring early diagnosis and appropriate management. Many individuals are unaware of their genetic risk until they or a family member are diagnosed with cancer. Educating both healthcare providers and the public about the signs and symptoms of this condition can lead to earlier interventions and better outcomes.
Support Networks
Living with Lynch Syndrome can be challenging, both emotionally and physically. Support networks, including patient advocacy groups and online communities, provide valuable resources and connections for individuals and families affected by this condition. These networks offer information, emotional support, and opportunities to participate in research studies.
Genetic Counseling
Genetic counseling plays a vital role in managing Lynch Syndrome. Counselors help individuals understand their genetic test results, assess their cancer risk, and make informed decisions about screening and preventive measures. They also guide family members through the process of genetic testing and risk assessment.
Research and Future Directions
Ongoing research is essential for advancing our understanding of Lynch Syndrome and improving outcomes for affected individuals. Scientists are exploring new ways to detect and treat cancers associated with this condition, as well as investigating potential therapies to target the underlying genetic mutations.
Emerging Therapies
Immunotherapy has shown promise in treating cancers linked to Lynch Syndrome. Because these cancers often have high levels of mutations, they may be more responsive to treatments that harness the immune system to attack tumor cells. Clinical trials are underway to evaluate the effectiveness of immunotherapy in this context.
Advances in Genetic Testing
Technological advancements are making genetic testing more accessible and affordable. Next-generation sequencing techniques allow for comprehensive analysis of multiple genes simultaneously, providing a clearer picture of an individual’s genetic risk. These innovations are paving the way for personalized medicine approaches tailored to each person’s unique genetic profile.