Leishmaniasis, often abbreviated as “Leish,” is a group of diseases caused by parasites belonging to the genus Leishmania. These diseases are prevalent in many parts of the world, particularly in tropical and subtropical regions. The condition manifests in various forms, including cutaneous, mucocutaneous, and visceral leishmaniasis, with the latter also known as Kala-Azar. This article explores the causes, symptoms, diagnosis, and treatment options for this complex disease.
Understanding the Causes of Leishmaniasis
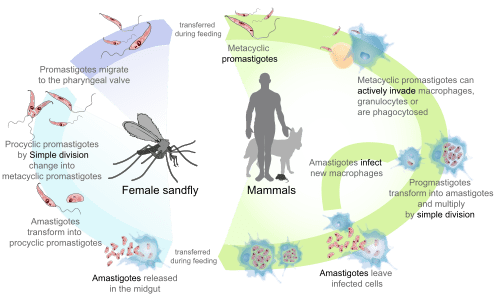
Leishmaniasis is caused by protozoan parasites that belong to the genus Leishmania. These parasites are transmitted to humans through the bite of infected female sandflies. Sandflies are small insects that thrive in warm climates and are most active during twilight hours. The lifecycle of the parasite involves two hosts: the sandfly and a mammalian host, which can include humans, dogs, and rodents.
The Role of Sandflies
- Sandflies become infected when they feed on the blood of an infected mammalian host.
- Once inside the sandfly, the parasites multiply and transform into a form capable of infecting another host.
- When the infected sandfly bites another mammal, it transmits the parasites into the bloodstream, leading to infection.
Environmental and Social Factors
Certain environmental and social factors increase the risk of transmission. Poor housing conditions, lack of proper sanitation, and deforestation create ideal breeding grounds for sandflies. Additionally, malnutrition and weakened immune systems make individuals more susceptible to severe forms of the disease, such as visceral leishmaniasis.
Recognizing the Symptoms of Leishmaniasis
The symptoms of leishmaniasis vary depending on the type of disease. Each form has distinct clinical manifestations, making accurate diagnosis critical for effective treatment.
Cutaneous Leishmaniasis
Cutaneous leishmaniasis is the most common form of the disease. It primarily affects the skin and is characterized by the following symptoms:
- Appearance of skin lesions or ulcers at the site of the sandfly bite.
- Lesions may take weeks or months to develop and often leave scars.
- In some cases, multiple lesions may appear, leading to disfiguration.
Mucocutaneous Leishmaniasis
Mucocutaneous leishmaniasis is a more severe form that affects both the skin and mucous membranes. Its symptoms include:
- Destruction of soft tissues in the nose, mouth, and throat.
- Progressive damage to the nasal septum, leading to deformities.
- Painful sores that can impair breathing and eating.
Visceral Leishmaniasis (Kala-Azar)
Visceral leishmaniasis, commonly referred to as Kala-Azar, is the most severe form of the disease. If left untreated, it is almost always fatal. Key symptoms include:
- Fever that persists for weeks or months.
- Significant weight loss and weakness.
- Enlargement of the spleen and liver.
- Anemia and low white blood cell count.
Diagnosing Leishmaniasis
Accurate diagnosis is essential for determining the appropriate treatment plan. Various methods are used to diagnose leishmaniasis, depending on the form of the disease.
Clinical Evaluation
A thorough clinical evaluation is the first step in diagnosing leishmaniasis. Healthcare providers assess the patient’s travel history, exposure to sandflies, and the presence of characteristic symptoms. However, clinical evaluation alone is insufficient for a definitive diagnosis.
Laboratory Tests
Several laboratory tests are available to confirm the presence of the parasite:
- Microscopic Examination: Tissue samples from skin lesions or bone marrow are examined under a microscope to identify the parasite.
- Serological Tests: Blood tests detect antibodies produced by the immune system in response to the infection.
- Molecular Techniques: Polymerase chain reaction (PCR) tests are highly sensitive and specific for detecting parasite DNA.
Differential Diagnosis
Because the symptoms of leishmaniasis overlap with other diseases, healthcare providers must rule out conditions such as malaria, tuberculosis, and lymphoma before confirming a diagnosis.
Treatment Options for Leishmaniasis
Treatment for leishmaniasis depends on the type of disease, its severity, and the patient’s overall health. Early diagnosis and prompt treatment are crucial to prevent complications and reduce mortality rates.
Treatment for Cutaneous Leishmaniasis
For localized cutaneous leishmaniasis, treatment may not always be necessary, as the lesions often heal on their own. However, medical intervention is recommended to prevent scarring and secondary infections. Common treatments include:
- Topical Medications: Antiparasitic creams or ointments applied directly to the lesions.
- Cryotherapy: Freezing the lesions with liquid nitrogen to destroy infected tissue.
- Systemic Drugs: Oral or injectable medications, such as pentavalent antimonials, for more severe cases.
Treatment for Mucocutaneous Leishmaniasis
Mucocutaneous leishmaniasis requires aggressive treatment due to its potential to cause permanent damage. Treatment options include:
- Intravenous Medications: Drugs like amphotericin B are administered to target the parasite effectively.
- Combination Therapy: A combination of antiparasitic drugs to enhance efficacy and reduce resistance.
- Surgical Intervention: In advanced cases, reconstructive surgery may be necessary to repair damaged tissues.
Treatment for Visceral Leishmaniasis (Kala-Azar)
Visceral leishmaniasis is a medical emergency and requires immediate treatment. The primary goal is to eliminate the parasite and manage complications. Treatment options include:
- Liposomal Amphotericin B: Considered the first-line treatment due to its high efficacy and safety profile.
- Pentavalent Antimonials: Used in regions where liposomal amphotericin B is unavailable.
- Supportive Care: Nutritional support, blood transfusions, and management of secondary infections.
Challenges in Treatment
Despite advances in treatment, several challenges remain:
- Drug Resistance: Some strains of the parasite have developed resistance to conventional medications.
- Cost and Accessibility: Effective treatments like liposomal amphotericin B are expensive and not widely available in endemic regions.
- Side Effects: Many antiparasitic drugs have significant side effects, requiring careful monitoring during treatment.
Preventing Leishmaniasis
Prevention plays a critical role in controlling the spread of leishmaniasis. Public health measures focus on reducing exposure to sandflies and managing reservoir hosts.
Vector Control
Efforts to control sandfly populations include:
- Use of insecticide-treated bed nets and indoor residual spraying.
- Elimination of breeding sites by improving sanitation and waste management.
- Community education on avoiding outdoor activities during peak sandfly activity times.
Vaccination and Research
While no vaccine is currently available for humans, ongoing research aims to develop effective preventive measures. Vaccines for animals, particularly dogs, have shown promise in reducing transmission in endemic areas.
Surveillance and Early Detection
Strengthening surveillance systems and ensuring early detection of cases are vital for controlling outbreaks. Rapid diagnostic tools and training for healthcare workers are essential components of these efforts.