Latex allergy, also known as an allergic reaction to natural rubber latex, is a growing concern in both medical and everyday settings. Referred to as LA in some medical literature, this condition affects individuals who come into contact with products made from natural rubber latex. While it may seem like a minor issue, the consequences of latex allergy can range from mild irritation to life-threatening reactions. Understanding its causes, recognizing its symptoms, and learning how to manage it effectively are crucial steps for those affected and those who care for them.
What Is Latex?
Latex is a natural product derived from the sap of rubber trees. It is widely used in the production of various items due to its flexibility, durability, and waterproof properties. Common products made from latex include gloves, balloons, condoms, medical devices, and even some clothing materials. Despite its utility, latex contains proteins that can trigger allergic reactions in certain individuals. These reactions occur when the immune system mistakenly identifies these proteins as harmful substances.
Causes of Latex Allergy
The development of latex allergy is primarily linked to repeated exposure to latex-containing products. The following factors contribute to the onset of this condition:
Occupational Exposure
- Healthcare workers frequently use latex gloves, making them more susceptible to developing an allergy over time.
- Individuals working in rubber manufacturing or processing industries are also at higher risk due to prolonged contact with latex materials.
Medical Procedures
- Patients undergoing multiple surgeries or medical procedures may develop sensitivity to latex due to repeated exposure to latex-based medical equipment.
- Children with spina bifida are particularly vulnerable because they often require frequent medical interventions involving latex products.
Cross-Reactivity with Certain Foods
- Some individuals with latex allergy experience allergic reactions to specific foods such as bananas, avocados, kiwis, and chestnuts. This phenomenon, known as cross-reactivity, occurs because these foods contain proteins similar to those found in latex.
Symptoms of Latex Allergy
The symptoms of latex allergy vary depending on the severity of the reaction and the mode of exposure. They can be classified into three main categories:
Contact Dermatitis
- This is the mildest form of latex allergy and typically affects the skin.
- Symptoms include redness, itching, swelling, and dryness in areas where the skin comes into contact with latex.
- These symptoms usually appear within hours after exposure and resolve within a few days.
Allergic Contact Dermatitis
- This type of reaction is caused by chemicals used in the manufacturing of latex products rather than the latex itself.
- Symptoms are similar to contact dermatitis but tend to be more severe and long-lasting.
- Blisters, crusting, and intense itching are common signs of this condition.
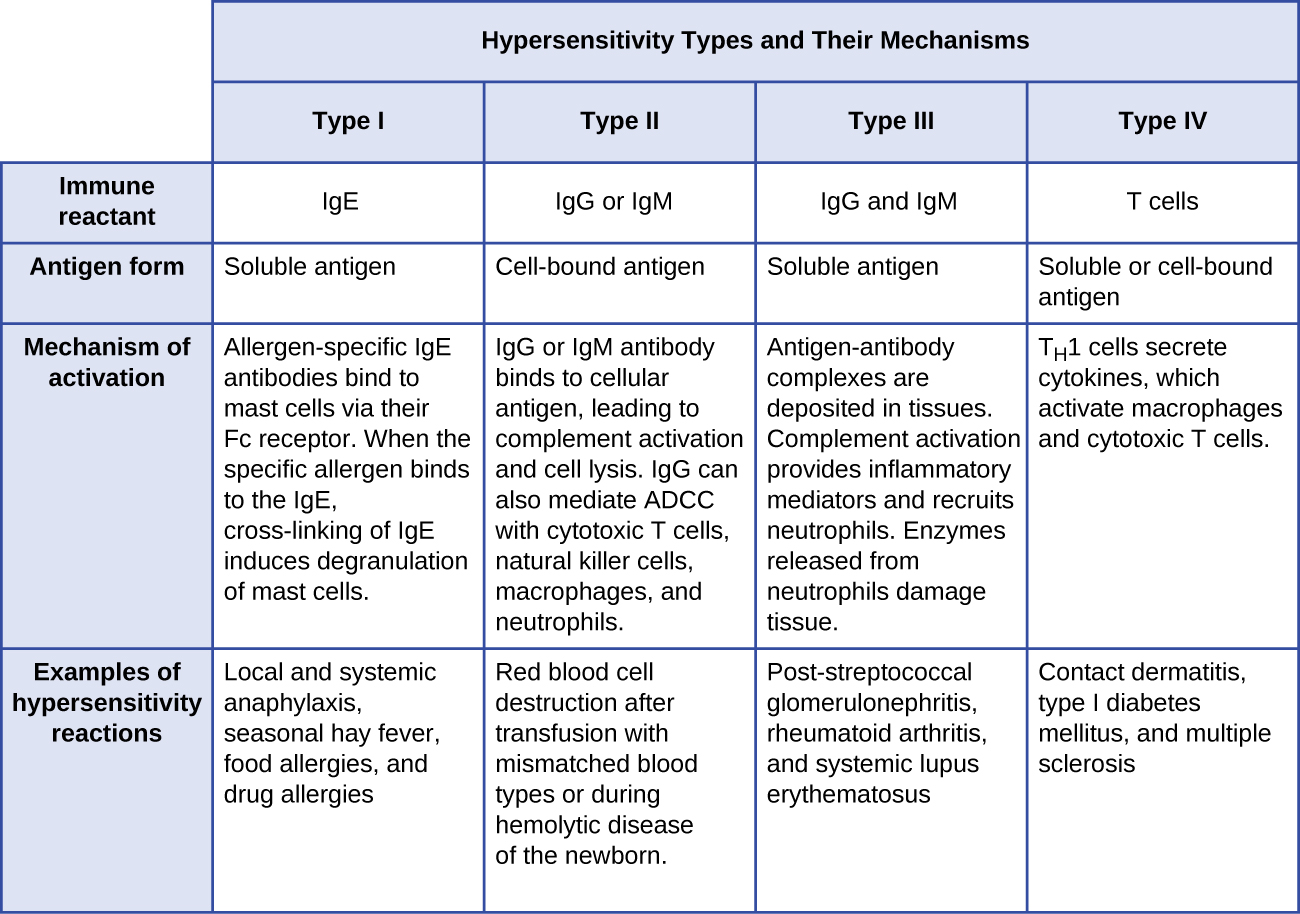
Immediate Hypersensitivity Reaction
- This is the most serious form of latex allergy and requires immediate medical attention.
- Symptoms can include hives, nasal congestion, difficulty breathing, rapid heartbeat, and swelling of the throat or tongue.
- In extreme cases, anaphylaxis—a potentially fatal reaction—can occur, leading to a drop in blood pressure and loss of consciousness.
Diagnosis of Latex Allergy
Identifying latex allergy involves a combination of patient history, physical examination, and specialized tests. Healthcare providers rely on the following methods to confirm a diagnosis:
Patient History
- Doctors ask about past exposure to latex products and any previous allergic reactions.
- Details about occupational hazards, medical procedures, and dietary habits help pinpoint potential triggers.
Skin Prick Test
- A small amount of latex extract is applied to the skin, usually on the forearm.
- If the individual is allergic, a raised bump or redness will appear at the test site within 15 to 20 minutes.
Blood Tests
- Blood samples are analyzed for the presence of immunoglobulin E antibodies specific to latex proteins.
- This test is less invasive than a skin prick test and is often used for individuals who cannot undergo skin testing due to severe skin conditions or medication use.
Management of Latex Allergy
While there is no cure for latex allergy, effective management strategies can minimize risks and improve quality of life. The key approaches include avoidance, substitution, and emergency preparedness.
Avoidance
- Individuals with latex allergy should avoid direct contact with latex-containing products whenever possible.
- Reading labels carefully and choosing latex-free alternatives is essential for reducing exposure.
- Informing healthcare providers about the allergy ensures that latex-free equipment is used during medical procedures.
Substitution
- Non-latex gloves made from materials like nitrile or vinyl are excellent alternatives for healthcare workers and others who require protective gear.
- Latex-free condoms and other personal care products are readily available in most markets.
- Switching to synthetic rubber or silicone-based items can significantly reduce the risk of allergic reactions.
Emergency Preparedness
- Individuals with severe latex allergy should carry an epinephrine auto-injector at all times to treat anaphylactic reactions promptly.
- Wearing a medical alert bracelet or necklace helps inform others of the allergy in case of emergencies.
- Developing an action plan with a healthcare provider ensures quick and appropriate responses during allergic episodes.
Prevention Strategies
Preventing latex allergy involves minimizing unnecessary exposure and promoting awareness among high-risk groups. Some practical measures include:
Education and Training
- Healthcare facilities should educate staff about the risks of latex allergy and encourage the use of non-latex products.
- Training programs can teach proper handling techniques to reduce the release of latex particles into the air.
Product Labeling
- Manufacturers should clearly label products containing latex to assist consumers in making informed choices.
- Regulatory bodies play a vital role in enforcing labeling standards and ensuring compliance across industries.
Research and Innovation
- Ongoing research aims to develop hypoallergenic latex products by modifying the proteins responsible for allergic reactions.
- Advancements in synthetic materials continue to provide safer alternatives for various applications.
Living with Latex Allergy
For those diagnosed with latex allergy, adapting to a latex-free lifestyle may initially seem challenging. However, with proper planning and support, it is entirely manageable. Here are some tips for navigating daily life:
Home Environment
- Replace household items like rubber bands, erasers, and latex-containing toys with non-latex versions.
- Use hypoallergenic bedding and mattress covers to prevent accidental exposure.
Dining Out
- Communicate your allergy to restaurant staff and inquire about food preparation practices.
- Avoid dishes that may have been prepared using latex gloves or utensils.
Travel and Social Activities
- Carry a list of safe and unsafe foods to share with hosts or chefs while traveling.
- Bring your own non-latex gloves or protective gear if participating in activities that might involve latex exposure.





