Knee effusion, commonly referred to as a swollen knee, is a condition that occurs when excess fluid accumulates in or around the knee joint. This can lead to discomfort, limited mobility, and even severe pain depending on the underlying cause. While the medical community often uses abbreviations like “OA” for osteoarthritis or “RA” for rheumatoid arthritis to describe potential causes, this article will focus on providing an in-depth understanding of knee effusion without relying on such shorthand.
Understanding Knee Effusion
The knee joint is one of the most complex joints in the human body, playing a critical role in movement and weight-bearing activities. When the joint becomes swollen due to an abnormal buildup of fluid, it is referred to as knee effusion. This swelling can result from a variety of factors, ranging from acute injuries to chronic conditions. Understanding the anatomy of the knee is essential to grasp why effusion occurs.
Anatomy of the Knee Joint
- Bones: The knee joint is formed by three bones: the femur (thighbone), the tibia (shinbone), and the patella (kneecap).
- Ligaments: These strong bands of tissue connect the bones and provide stability to the joint.
- Cartilage: A smooth tissue called articular cartilage covers the ends of the bones, allowing them to glide smoothly against each other.
- Synovial Membrane: This lining produces synovial fluid, which lubricates the joint and reduces friction during movement.
When the synovial membrane becomes inflamed or damaged, it can produce excess fluid, leading to knee effusion.
Common Causes of Knee Effusion
Knee effusion can be caused by a wide range of factors, including injuries, infections, and systemic diseases. Identifying the underlying cause is crucial for effective treatment.
Injuries
Injuries are among the most common causes of knee effusion. These can occur during sports activities, accidents, or even simple falls. Some examples include:
- Ligament Tears: Injuries to the anterior cruciate ligament or posterior cruciate ligament can lead to significant swelling.
- Meniscus Tears: Damage to the cartilage within the knee joint can cause fluid accumulation.
- Fractures: Broken bones around the knee can irritate the joint and trigger swelling.
- Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion the joint, can also result in effusion.
Infections
Infections in the knee joint, though less common, can lead to rapid and severe swelling. These infections may arise from bacteria entering the joint through a wound or spreading from another part of the body. Septic arthritis is a serious condition that requires immediate medical attention.
Chronic Conditions
Several long-term health issues can contribute to knee effusion:
- Osteoarthritis: This degenerative joint disease causes the cartilage to break down, leading to inflammation and fluid buildup.
- Rheumatoid Arthritis: An autoimmune disorder where the immune system attacks the joints, causing inflammation and swelling.
- Gout: A form of arthritis caused by the buildup of uric acid crystals in the joint.
- Pseudogout: Similar to gout but caused by calcium pyrophosphate crystals.
Other Causes
Less common causes of knee effusion include tumors, cysts, and bleeding disorders. In rare cases, certain medications can also lead to joint swelling as a side effect.
Symptoms of Knee Effusion
The symptoms of knee effusion can vary depending on the severity and underlying cause. However, some common signs include:
- Visible Swelling: The knee may appear larger than usual and feel tight or puffy.
- Pain: Discomfort or sharp pain, especially during movement or pressure on the joint.
- Stiffness: Difficulty bending or straightening the knee.
- Redness and Warmth: The skin over the knee may feel warm to the touch and appear red.
- Instability: A feeling that the knee might give way or buckle.
In cases of infection or severe injury, additional symptoms such as fever, chills, or extreme pain may occur, indicating the need for urgent medical care.
Diagnosis of Knee Effusion
Proper diagnosis is essential to determine the cause of knee effusion and guide treatment decisions. Healthcare providers typically use a combination of physical examination, imaging tests, and laboratory analyses to identify the underlying issue.
Physical Examination
A doctor will assess the knee by looking for visible swelling, checking for warmth or redness, and testing the range of motion. They may also ask about recent injuries, activities, or symptoms to narrow down potential causes.
Imaging Tests
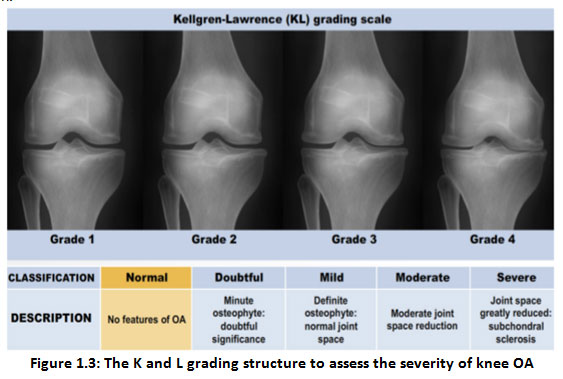
Imaging techniques such as X-rays, magnetic resonance imaging, and ultrasounds can help visualize the structures within the knee and identify abnormalities like fractures, ligament tears, or cartilage damage.
Joint Aspiration
In some cases, a procedure called joint aspiration may be performed. This involves removing a small sample of the fluid from the knee joint using a needle. The fluid is then analyzed in a laboratory to check for signs of infection, inflammation, or crystal deposits.
Treatment Options for Knee Effusion
Treatment for knee effusion depends on the underlying cause and the severity of the condition. In many cases, a combination of approaches is used to alleviate symptoms and address the root problem.
Rest and Activity Modification
One of the first steps in managing knee effusion is reducing stress on the joint. This may involve avoiding activities that exacerbate the swelling, such as running or jumping, and using assistive devices like crutches to limit weight-bearing.
Ice and Compression
Applying ice packs to the knee for 15-20 minutes several times a day can help reduce swelling and numb pain. Compression bandages or knee braces may also be used to provide support and minimize fluid buildup.
Medications
Over-the-counter pain relievers such as ibuprofen or acetaminophen can help manage pain and inflammation. In cases of infection or autoimmune conditions, prescription medications like antibiotics or corticosteroids may be necessary.
Physical Therapy
Physical therapy exercises can strengthen the muscles around the knee, improve flexibility, and promote healing. A therapist may also use techniques like ultrasound or electrical stimulation to reduce swelling.
Drainage Procedures
For severe cases of knee effusion, a healthcare provider may recommend draining the excess fluid using a needle. This procedure, known as arthrocentesis, can provide immediate relief and allow for further analysis of the fluid.
Surgical Interventions
In cases where conservative treatments fail or the underlying cause requires surgical correction, procedures such as arthroscopy or joint replacement surgery may be considered. Arthroscopy involves inserting a small camera into the joint to repair damaged tissues, while joint replacement is typically reserved for advanced arthritis.
Preventing Knee Effusion
While not all cases of knee effusion can be prevented, certain measures can reduce the risk of developing this condition:
- Maintain a Healthy Weight: Excess weight places added stress on the knees, increasing the likelihood of joint problems.
- Exercise Regularly: Strengthening the muscles around the knee can provide better support and stability.
- Use Proper Techniques: Whether playing sports or lifting heavy objects, using correct form can prevent injuries.
- Wear Protective Gear: During high-impact activities, wearing knee pads or braces can protect the joint from trauma.
By understanding the causes, symptoms, and treatments of knee effusion, individuals can take proactive steps to manage their joint health and seek timely medical care when needed.