Keratoacanthoma, often abbreviated as KA, is a relatively common yet intriguing skin condition that poses diagnostic and therapeutic challenges. While it may resemble squamous cell carcinoma in appearance, keratoacanthoma typically follows a distinct course, often resolving on its own without intervention. However, due to its potential for rapid growth and resemblance to more aggressive forms of skin cancer, understanding this condition is essential for both patients and healthcare providers.
What Is Keratoacanthoma?
Keratoacanthoma is a type of skin lesion that usually appears as a rapidly growing, dome-shaped bump with a central crater filled with keratin, a protein found in the outer layer of the skin. This lesion typically develops over a few weeks to months and can occur anywhere on the body, though it most commonly affects sun-exposed areas such as the face, neck, arms, and hands. While keratoacanthoma is generally considered benign, its clinical behavior and microscopic features sometimes overlap with those of squamous cell carcinoma, making accurate diagnosis critical.
Types of Keratoacanthoma
- Solitary Keratoacanthoma: The most common form, characterized by a single lesion.
- Multiple Keratoacanthomas: Occurs when several lesions develop simultaneously, often associated with underlying conditions like Muir-Torre syndrome or exposure to certain medications.
- Keratoacanthoma Centrifugum Marginatum: A rare variant that grows outward in a ring-like pattern.
Causes of Keratoacanthoma
The exact cause of keratoacanthoma remains unclear, but several factors are believed to contribute to its development. Understanding these causes can help individuals take preventive measures and reduce their risk.
Sun Exposure
Prolonged and excessive exposure to ultraviolet radiation from the sun is one of the primary risk factors for developing keratoacanthoma. Ultraviolet rays can damage the DNA in skin cells, leading to abnormal growth patterns. People who spend significant time outdoors or use tanning beds frequently are at higher risk.
Genetic Factors
Some individuals may have a genetic predisposition to developing keratoacanthoma. Certain inherited conditions, such as Muir-Torre syndrome, increase the likelihood of developing multiple keratoacanthomas. Additionally, mutations in specific genes involved in cell growth regulation may play a role in the formation of these lesions.
Immune System Suppression
Individuals with weakened immune systems, such as organ transplant recipients or those undergoing chemotherapy, are more susceptible to developing keratoacanthoma. A compromised immune system may fail to regulate abnormal cell growth effectively, allowing these lesions to form.
Trauma or Injury to the Skin
Physical trauma, such as cuts, burns, or surgical scars, can sometimes trigger the development of keratoacanthoma at the site of injury. This phenomenon suggests that local tissue damage may play a role in initiating the growth of these lesions.
Symptoms of Keratoacanthoma
Keratoacanthoma typically presents with distinctive symptoms that set it apart from other skin conditions. Recognizing these signs early can facilitate prompt diagnosis and treatment.
Rapid Growth
One of the hallmark features of keratoacanthoma is its rapid growth. These lesions can grow significantly within a matter of weeks, reaching sizes of up to several centimeters in diameter. This rapid expansion often prompts individuals to seek medical attention.
Dome-Shaped Appearance
Keratoacanthoma lesions are typically dome-shaped with a smooth, shiny surface. As the lesion matures, a central crater filled with keratin develops, giving it a characteristic “volcano-like” appearance. This feature is often key to differentiating keratoacanthoma from other types of skin growths.
Painless Nature
In most cases, keratoacanthoma does not cause pain unless it becomes ulcerated or infected. However, some individuals may experience mild discomfort or itching around the lesion.
Location
These lesions are most commonly found on sun-exposed areas of the body, such as the face, ears, scalp, neck, forearms, and hands. Their location often correlates with areas that receive frequent sun exposure.
Diagnosis of Keratoacanthoma
Accurate diagnosis of keratoacanthoma is crucial because of its resemblance to squamous cell carcinoma. Misdiagnosis can lead to unnecessary treatments or delays in addressing potentially malignant conditions.
Clinical Examination
A dermatologist will begin by conducting a thorough physical examination of the lesion. They will assess its size, shape, color, and texture, as well as inquire about its growth pattern and duration. The presence of a central keratin-filled crater is a strong indicator of keratoacanthoma.
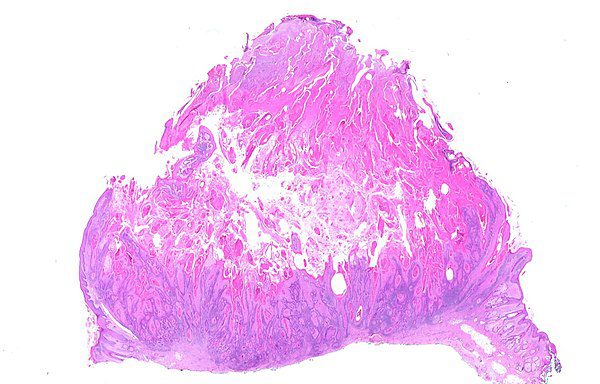
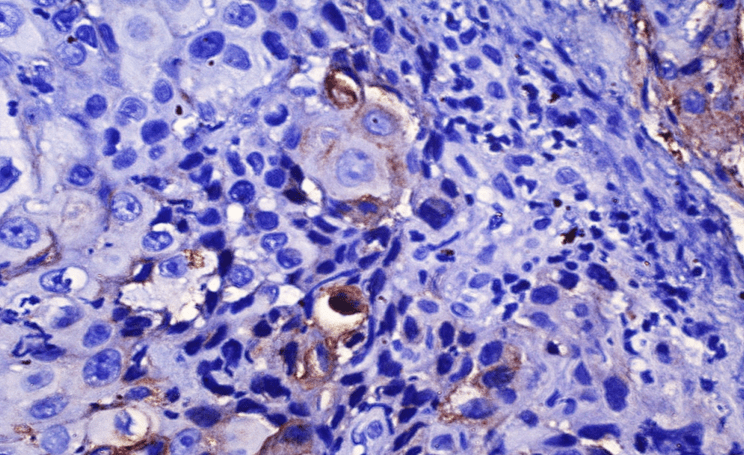
Biopsy
A biopsy is the gold standard for diagnosing keratoacanthoma. During this procedure, a small sample of the lesion is removed and examined under a microscope. Histopathological analysis reveals characteristic features, such as a well-differentiated squamous epithelium lining the crater and a central core of keratin.
Dermoscopy
Dermoscopy is a non-invasive technique that uses a specialized magnifying device to examine the lesion’s surface and subsurface structures. This tool can help differentiate keratoacanthoma from other skin conditions based on specific patterns and colors observed during the examination.
Imaging Studies
In cases where the lesion appears deep or invasive, imaging studies such as ultrasound or magnetic resonance imaging may be performed to evaluate the extent of involvement and rule out metastasis.
Treatment Options for Keratoacanthoma
While some keratoacanthomas resolve spontaneously, treatment is often recommended to prevent complications, ensure proper healing, and rule out malignancy. Several treatment options are available, depending on the size, location, and characteristics of the lesion.
Surgical Excision
Surgical removal is the most common and effective treatment for keratoacanthoma. This procedure involves cutting out the entire lesion along with a margin of healthy tissue to ensure complete removal. Surgical excision provides definitive results and allows for histopathological examination of the excised tissue.
Curettage and Electrodessication
This minimally invasive technique involves scraping away the lesion with a curette and then using an electric current to destroy any remaining abnormal cells. Curettage and electrodessication are suitable for smaller lesions and offer good cosmetic outcomes.
Cryotherapy
Cryotherapy involves freezing the lesion with liquid nitrogen to destroy abnormal cells. This method is particularly useful for superficial keratoacanthomas and is associated with minimal scarring. However, it may require multiple sessions for complete resolution.
Laser Therapy
Laser therapy uses focused beams of light to target and remove the lesion. This approach is ideal for cosmetically sensitive areas, such as the face, as it minimizes scarring and promotes faster healing.
Topical Treatments
In certain cases, topical medications such as imiquimod cream may be prescribed to stimulate the immune system to attack the lesion. While effective for some patients, this option requires prolonged application and close monitoring.
Observation
For select cases of keratoacanthoma that are small, asymptomatic, and located in low-risk areas, observation may be an acceptable approach. Regular follow-up visits are necessary to monitor for changes in size, appearance, or behavior.
Prevention of Keratoacanthoma
While not all cases of keratoacanthoma can be prevented, adopting certain lifestyle changes and protective measures can significantly reduce the risk of developing this condition.
Sun Protection
Limiting sun exposure, especially during peak hours, wearing protective clothing, and applying broad-spectrum sunscreen regularly are essential steps to minimize ultraviolet radiation damage to the skin.
Regular Skin Checks
Performing self-examinations of the skin and scheduling routine check-ups with a dermatologist can help detect suspicious lesions early. Early detection increases the likelihood of successful treatment and reduces the risk of complications.
Avoiding Risk Factors
Minimizing exposure to known risk factors, such as smoking, excessive alcohol consumption, and immunosuppressive medications, can lower the chances of developing keratoacanthoma.
Healthy Lifestyle
Maintaining a balanced diet, staying physically active, and managing stress levels contribute to overall health and support the immune system’s ability to fight off abnormal cell growth.